- Record: found
- Abstract: found
- Article: found
Nab-paclitaxel plus gemcitabine for metastatic pancreatic adenocarcinoma after Folfirinox failure: an AGEO prospective multicentre cohort
Read this article at
Abstract
Background:
There is currently no standard second-line treatment for metastatic pancreatic adenocarcinoma (MPA), and progression-free survival is consistently <4 months in this setting. The aim of this study was to evaluate the efficacy and tolerability of Nab-paclitaxel plus gemcitabine (A+G) after Folfirinox failure in MPA.
Methods:
From February 2013 to July 2014, all consecutive patients treated with A+G for histologically proven MPA after Folfirinox failure were prospectively enrolled in 12 French centres. A+G was delivered as described in the MPACT trial, until disease progression, patient refusal or unacceptable toxicity.
Results:
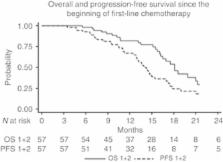
Fifty-seven patients were treated with Nab-paclitaxel plus gemcitabine, for a median of 4 cycles (range 1–12). The disease control rate was 58%, with a 17.5% objective response rate. Median overall survival (OS) was 8.8 months (95% CI: 6.2–9.7) and median progression-free survival was 5.1 months (95% CI: 3.2–6.2). Since the start of first-line chemotherapy, median OS was 18 months (95% CI: 16–21). No toxic deaths occurred. Grade 3–4 toxicities were reported in 40% of patients, consisting of neutropenia (12.5%), neurotoxicity (12.5%), asthenia (9%) and thrombocytopenia (6.5%).
Related collections
Most cited references15
- Record: found
- Abstract: found
- Article: not found
EUROCARE-4. Survival of cancer patients diagnosed in 1995-1999. Results and commentary.
- Record: found
- Abstract: found
- Article: not found
Peripheral neuropathy induced by paclitaxel: recent insights and future perspectives.
- Record: found
- Abstract: found
- Article: not found