- Record: found
- Abstract: found
- Article: found
Predictors of person-centered maternity care: the role of socioeconomic status, empowerment, and facility type
Read this article at
Abstract
Background
Low use of maternal health services, as well as poor quality care, contribute to the high maternal mortality in sub-Saharan Africa (SSA). In particular, poor person-centered maternity care (PCMC), which captures user experience, contributes both directly to pregnancy outcomes and indirectly through decreased demand for services. While many studies have examined disparities in use of maternal health services, few have examined disparities in quality of care, and none to our knowledge has empirically examined disparities in PCMC in SSA. The aim of this study is to examine factors associated with PCMC, particularly the role of household wealth, personal empowerment, and type of facility.
Methods
Data are from a survey conducted in western Kenya in 2016, with women aged 15 to 49 years who delivered in the 9 weeks preceding the survey ( N = 877). PCMC is operationalized as a summative score based on responses to 30 items in the PCMC scale capturing dignity and respect, communication and autonomy, and supportive care.
Results
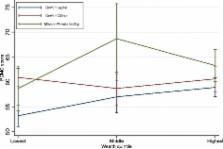
We find that net of other factors; wealthier, employed, literate, and married women report higher PCMC than poorer, unemployed, illiterate, and unmarried women respectively. Also, women who have experienced domestic violence report lower PCMC than those who have never experienced domestic violence. In addition, women who delivered in health centers and private facilities reported higher PCMC than those who delivered in public hospitals. The effect of employment and facility type is conditional on wealth, and is strongest for the poorest women. Poor women who are unemployed and poor women who deliver in higher-level facilities receive the lowest quality PCMC.
Related collections
Most cited references34

- Record: found
- Abstract: found
- Article: found
Drivers and deterrents of facility delivery in sub-Saharan Africa: a systematic review
- Record: found
- Abstract: found
- Article: found
Factors associated with the use and quality of antenatal care in Nepal: a population-based study using the demographic and health survey data
- Record: found
- Abstract: found
- Article: not found