- Record: found
- Abstract: found
- Article: found
Modest Elevation in BNP in Asymptomatic Hypertensive Patients Reflects Sub-Clinical Cardiac Remodeling, Inflammation and Extracellular Matrix Changes
Read this article at
Abstract
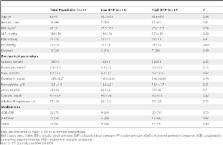
In asymptomatic subjects B-type natriuretic peptide (BNP) is associated with adverse cardiovascular outcomes even at levels well below contemporary thresholds used for the diagnosis of heart failure. The mechanisms behind these observations are unclear. We examined the hypothesis that in an asymptomatic hypertensive population BNP would be associated with sub-clinical evidence of cardiac remodeling, inflammation and extracellular matrix (ECM) alterations. We performed transthoracic echocardiography and sampled coronary sinus (CS) and peripheral serum from patients with low (n = 14) and high BNP (n = 27). Peripheral BNP was closely associated with CS levels (r = 0.92, p<0.001). CS BNP correlated significantly with CS levels of markers of collagen type I and III turnover including: PINP (r = 0.44, p = 0.008), CITP (r = 0.35, p = 0.03) and PIIINP (r = 0.35, p = 0.001), and with CS levels of inflammatory cytokines including: TNF-α (r = 0.49, p = 0.002), IL-6 (r = 0.35, p = 0.04), and IL-8 (r = 0.54, p<0.001). The high BNP group had greater CS expression of fibro-inflammatory biomarkers including: CITP (3.8±0.7 versus 5.1±1.9, p = 0.007), TNF-α (3.2±0.5 versus 3.7±1.1, p = 003), IL-6 (1.9±1.3 versus 3.4±2.7, p = 0.02) and hsCRP (1.2±1.1 versus 2.4±1.1, p = 0.04), and greater left ventricular mass index (97±20 versus 118±26 g/m 2, p = 0.03) and left atrial volume index (18±2 versus 21±4, p = 0.008). Our data provide insight into the mechanisms behind the observed negative prognostic impact of modest elevations in BNP and suggest that in an asymptomatic hypertensive cohort a peripheral BNP measurement may be a useful marker of an early, sub-clinical pathological process characterized by cardiac remodeling, inflammation and ECM alterations.
Related collections
Most cited references33
- Record: found
- Abstract: found
- Article: not found
Rapid measurement of B-type natriuretic peptide in the emergency diagnosis of heart failure.
- Record: found
- Abstract: found
- Article: not found
2003 World Health Organization (WHO)/International Society of Hypertension (ISH) statement on management of hypertension.
- Record: found
- Abstract: found
- Article: not found