- Record: found
- Abstract: found
- Article: found
Radiation dose escalation for loco-regional recurrence of breast cancer after mastectomy
Read this article at
Abstract
Background
Radiation is a standard component of treatment for patients with locoregional recurrence (LRR) of breast cancer following mastectomy. The current study reports the results of a 10% radiation dose escalation in these patients.
Methods
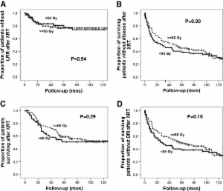
159 patients treated at MD Anderson Cancer Center between 1994-2006 with isolated LRR after mastectomy alone were reviewed. Patients in the standard treatment group (65 pts, 40.9%) were treated to 50 Gy comprehensively plus a boost of 10 Gy. The dose escalated group (94 pts, 59.1%) was treated to 54 Gy comprehensively and a minimum 12 Gy boost. Median dose in the standard dose and dose escalated group was 60 Gy (±1 Gy, 95% CI) and 66 Gy (±0.5 Gy, 95% CI) respectively. Median follow up for living patients was 94 months from time of recurrence.
Results
The actuarial five year locoregional control (LRC) rate was 77% for the entire study population. The five year overall survival and disease-free survival was 55% and 41%, respectively. On multivariate analysis, initial tumor size (p = 0.03), time to initial LRR (p = 0.03), absence of gross tumor at the time of radiation (p = 0.001) and Her2 status (p = 0.03) were associated with improved LRC. Five year LRC rates were similar in patients with a complete response to chemotherapy without surgery and patients with a complete surgical excision (77% vs 83%, p = NS), compared to a 63% LRC rate in patients with gross disease at the time of radiation (p = 0.024). LRC rates were 80% in the standard dose group and 75% in the dose escalated group (p = NS).
Conclusions
While LRR following mastectomy is potentially curable, distant metastasis and local control rates remain suboptimal. Radiation dose escalation did not appear to improve LRC. Given significant local failure rates, these patients are good candidates for additional strategies to improve their outcomes.
Related collections
Most cited references19
- Record: found
- Abstract: found
- Article: not found
Loco-regional recurrence after mastectomy in high-risk breast cancer--risk and prognosis. An analysis of patients from the DBCG 82 b&c randomization trials.
- Record: found
- Abstract: found
- Article: not found