- Record: found
- Abstract: found
- Article: found
Postoperative clinical outcomes with and without short-term intravenous tranexamic acid after posterior lumbar interbody fusion: A prospective cohort study
Read this article at
Abstract
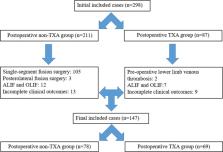
The use of tranexamic acid (TXA) in posterior lumbar interbody fusion (PLIF) surgery is believed to be beneficial for reducing intraoperative blood loss, postoperative drainage volume (PDV), and length of hospital stay (LOS). However, whether continued administration of intravenous TXA within 24 hours after surgery is more beneficial to patients has not yet been studied. This study prospectively analyzed the perioperative outcomes of patients who received and did not receive intravenous TXA within 24 hours after PLIF (≥2 segments) surgery from January 2018 to December 2021. A total of 78 and 69 patients were included in the TXA (receive intravenous TXA intraoperatively and within 24 hours postoperatively) and non-TXA (only receive intravenous TXA intraoperatively) groups, respectively. No significant differences were observed in the intraoperative blood loss and operative time between the 2 groups. The postoperative drainage volume, postoperative drainage time, and length of hospital stay in the TXA group were significantly lower than those in the non-TXA group. The rates and volumes of postoperative blood and albumin transfusions were significantly lower in the TXA group than those in the non-TXA group. No significant differences were observed in the perioperative complication rates between the 2 groups. No increase in thrombosis-related complications was observed with postoperative TXA administration. Short-term TXA use after PLIF (≥2 segments) surgery is safe. In addition to intraoperative use of TXA, additionally administration of intravenous TXA within 24 hours postoperatively can improve the perioperative clinical outcomes of patients without increasing the risk of thrombotic events.
Related collections
Most cited references44
- Record: found
- Abstract: found
- Article: not found
Lumbar interbody fusion: techniques, indications and comparison of interbody fusion options including PLIF, TLIF, MI-TLIF, OLIF/ATP, LLIF and ALIF.
- Record: found
- Abstract: not found
- Article: not found
The Roland-Morris Disability Questionnaire and the Oswestry Disability Questionnaire.
- Record: found
- Abstract: found
- Article: not found