- Record: found
- Abstract: found
- Article: found
Effect of Thrombotic Microangiopathy on Clinical Outcomes in Indian Patients With Lupus Nephritis
Read this article at
Abstract
Introduction
In addition to glomerular lesion, renal vascular lesion is also an important prognostic marker of lupus nephritis (LN). Among patients with various vascular changes, individuals with thrombotic microangiopathy (TMA) present with severe clinical manifestations and have a high mortality. The aim of the present study was to assess the spectrum and impact of TMA on the outcomes of LN. In a prospective observational study of 2.5 years’ duration, clinical and renal histopathological data regarding biopsy-proven LN were noted, and evaluation for antiphospholipid syndrome (APS) as a cause of TMA in LN was also carried out.
Methods
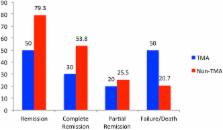
Study subjects were followed up actively for 6 months, and various outcomes were noted. Cases were divided into 2 groups as LN with TMA and LN without TMA, and various features were compared between the 2 groups. Outcomes recorded were complete response (CR), partial response (PR), treatment failure, and death.
Results
Of the 197 patients with LN, 50 patients (25.4%) were diagnosed with co-existing renal TMA. Five patients (10%) were found to have concomitant APS. As compared to patients without TMA, those with TMA had significantly higher rates of oliguria ( P = 0.035), advanced renal injury, that is, serum creatinine > 3mg/dl ( P = 0.002), fibrocellular and fibrous crescents ( P = 0.01), and tubular atrophy ( P = 0.001). Outcomes included CR in 15 patients (30%), PR in 10 (20%), failure in 19 (38%), and death in 6 (12%). Patients with LN with TMA had higher rates of treatment failure ( P = 0.02) compared to the group without TMA.
Related collections
Most cited references11
- Record: found
- Abstract: not found
- Article: not found
Renal vascular complications of systemic lupus erythematosus.
- Record: found
- Abstract: found
- Article: not found
Thrombotic microangiopathy in systemic lupus erythematosus: a cohort study in North Taiwan.
- Record: found
- Abstract: found
- Article: not found