- Record: found
- Abstract: found
- Article: found
Continuity of care in the approach to cardiac patients: from theory to practice/Continuidad asistencial en el abordaje del paciente cardiaco: de la teoría a la práctica
abstract
Read this article at
There is no author summary for this article yet. Authors can add summaries to their articles on ScienceOpen to make them more accessible to a non-specialist audience.
Abstract
Introduction
The Department of Cardiology of our hospital has a catchment population of 135,000
people. Until 2005, the relationship between the various levels of care (primary care,
and secondary and tertiary hospitals) was incidental. Patients were seen at different
levels of care and complementary tests were duplicated due to the lack of connections
between these levels, with all the implications this has for patients, quite apart
from the associated costs for the health service.
In 2005, the CSI HGH took charge of cardiology care in the catchment area, integrating
the outpatient cardiology care of five primary care (PC) health districts (Florida
Norte, Florida Sur, Pubilla Cases, Collblanc and Torrasa). In the first year, 12,000
appointments were carried out. The first intervention put into place was to transfer
the care of all the monitored patients with no identified heart disease or with only
minor conditions to PC. With this step, we managed to reduce the number of visits
to specialists of the Department of Cardiology by 30% in two years. Another intervention
was introduced in 2007: the establishment of clinical sessions bringing together professionals
of the Department of Cardiology and PC. A cardiologist was appointed for referral
of non-complex chronic heart patients and for advising primary care colleagues. Despite
all this, the response was not consistent across PC, so we proposed to segment the
cardiology care offer, according to the needs of our internal client, that is, primary
care.
Description of the intervention
The objective was to redefine cardiac care processes towards patient-based care through
a model of care that provides specialised care tailored to the needs of the ‘client’
within the care system as well as of patients. The intervention involved:
Establishment of an integrated care plan (ICP) to guide the approach to patients with
heart failure:
Establishment of a single appointment for diagnosis of heart failure (HF), including
tests and preparation of the care plan
Standardise response times for carrying out complementary tests
Introduce congestive heart failure (CHF) nurse case managers
Establish mechanisms for communication with PC that compensate for the lack of shared
medical records
Agree with PC the criteria for patient referral, as well which area of the hospital
patients should be sent to
Agree on the essential data required across the various levels of care
Establish a set of indicators for monitoring the criteria for referral, the volume
of activity in the various areas, and the time patients take to progress along the
care pathway
Setting up of a high-resolution cardiac imaging unit (CIU), establishing an agreed
number of processes and standard time (1 week) for performing of tests at the hospital
level.
Agree with PC on the types of cases that could benefit from a visit to this unit (appointment
with the nurse manager, electrocardiogram, echocardiogram, ± plain radiography)
Setting up of a service of virtual consultations for minor conditions and queries
from PC professionals, for cases in which a visit to the cardiologist is not required.
Define the activities and duties of the professionals of each level of care in relation
to each care process.
Results
1. The various interventions in place up to 2010 led to a 50% reduction in annual
outpatient consultations (2365 first appointments, 4538 follow-ups) and increased
the capacity of PC to deal with cardiac conditions, achieving a follow-up to first
appointment ratio of 1.92 in cardiology and waiting times for specialists of less
than a week.
2. Outcomes of the ICP and referrals for rapid diagnosis of CHF from March 2010 to
July 2011: Overall, 112 patients ranging from 43 to 90 years of age have been assessed
(Table 1).
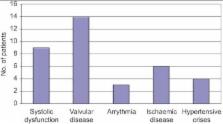
Of the patients examined, HF was confirmed in 36 cases and the underlying causes are
detailed in Figure 1.
3. Outcomes of the high-resolution CIU from June to July 2011: A total of 20 patients
were assessed. Patient age ranged from 25 to 88 years old, with 9 patients being octogenarians.
The reasons for the referral are listed in Table 2.
The outcomes with respect to the achievement of diagnosis for the processes that had
been the reason for the consultation are reported in Figure 2.
4. Outcomes of the virtual consultations: Over a period of three months, 34 consultations
were carried out and, of these, 32 have were resolved virtually. It was only considered
necessary for two patients to attend appointments in person to be assessed (in the
high-resolution CIU or at a conventional specialist appointment).
Discussion
Until 2005, the relationship between levels of care was incidental. Despite the fact
that there were significant initiatives between primary and specialised care, well
received by the latter, a direct connection had not developed between levels of care.
Since the time cardiology care came under the responsibility of our hospital, a series
of interventions have been put in place in order to agree with primary care, as well
as within tertiary care, pathways and criteria for action in line with clinical practice
guidelines to provide continuity of care to patients regardless of the level of care
where they are treated.
Conclusions
Consensus among the various different levels of care involved in the process, from
a client-provider (PC-Hospital) perspective, is essential to determine, on the basis
of care needs and the principle of subsidiarity, who does what and where.
With the establishment of new practices in integrated patient care, we aim to respond
to the care processes that are the reason for consultations quickly and efficiently.
Our vision is to develop a cardiology unit capable of adapting its responses to care
process requirements as requested by its internal client.
Conference abstract Spanish
Introducción
El servicio de cardiología de nuestro hospital da cobertura a una población total
de 135.000 habitantes. Hasta el año 2005 la relación entre los diferentes niveles
asistenciales (primaria, hospitales de 2° y 3er nivel) eran circunstanciales. El paciente
acudía a los diferentes niveles y se producía una duplicidad de exploraciones complementarias,
como consecuencia de la falta de conexión, con las implicaciones que conlleva para
el paciente y el gasto sanitario.
En el año 2005 el C.S.I-HGH se hace cargo de la Atención Cardiológica (AC) del área
de referencia, integrando la AC ambulatoria de cinco áreas básicas de Atención Primaria
(AP) (Florida Norte, Florida Sur, Pubilla Cases, Collblanc y Torrasa). En el primer
año se realizaron 12.000 visitas. La primera intervención que se realizó fue remitir
a AP el 100% de los pacientes controlados que no tenían patología cardiaca o con patología
banal. Con esta intervención se consigue en 2 años, reducir un 30% las visitas de
cardiología. A partir del 2007 se realiza una segunda intervención, que es la creación
de sesiones conjuntas entre el servicio de cardiología y la AP. Se crea el cardiólogo
referente para poder derivar a los pacientes cardiópatas crónicos no complejos y la
orientación al cliente interno. A pesar de todo, la respuesta por parte de la AP no
es homogénea, por lo que nos planteamos segmentar adecuadamente nuestra oferta asistencial
cardiológica a las necesidades de nuestro cliente interno Atención Primaria.
Descripción de la intervención
El objetivo de la intervención es redefinir los procesos asistenciales cardiológicos,
poniendo en el eje central al paciente a través de un modelo asistencial que dé respuesta
especializada a la necesidad del nivel asistencial ‘cliente’ y del paciente.
La intervención supuso (2010):
Puesta en marcha de un Plan Asistencial Integrado (PAI) para el abordaje de los pacientes
con Insuficiencia Cardiaca: Creación de un dispositivo de visita única para el diagnóstico
de Insuficiencia Cardiaca (IC)
Estandarizar tiempos de respuesta para la realización de pruebas complementarias
Implementar enfermera gestora de la insuficiencia cardiaca congestiva (ICC)
Instaurar sistemas de comunicación con la AP, que compensen la falta de una historia
clínica unificada.
Acordar con la AP criterios de derivación de pacientes y el dispositivo hospitalario
al cual remitir al paciente.
Acordar la información imprescindible entre los diferentes niveles asistenciales.
Implantar un sistema de indicadores para el seguimiento de los criterios de derivación,
el volumen de actividades de las diferentes áreas, y el tiempo de ciclo del proceso
Puesta en marcha de una Unidad de Alta Resolución (UAR) para patología cardíaca, establecimiento
de un número de procesos acordados y estandarización de los tiempos (1 semana) para
las exploraciones a nivel hospitalario.
Definir de forma consensuada con AP los procesos que se pueden beneficiar de una visita
de alta resolución (visita enfermera gestora, electrocardiograma, ecocardiograma,
± radiología simple)
Puesta en marcha de un servicio de consultaría no presencial para patología banal
y dudas por parte de la AP que no requiera visita presencial por parte del cardiólogo.
Definir las actividades y responsabilidades de cada nivel asistencial en base a cada
proceso.
Resultados
1. Las diferentes intervenciones hasta el 2010, han permitido disminuir la actividad
ambulatoria anual inicial en un 50% (2.365 primeras visitas, 4.538 segundas visitas),
incrementar la capacidad resolutiva de la AP en patología cardíaca, conseguir una
tasa de reiteración en las consultas de cardiología de 1,92, y ser accesibles en <1
semana.
2. Resultados PAI + derivaciones a diagnóstico rápido ICC en el periodo comprendido
entre marzo 2010 y julio 2011: Se han valorado un total de 112 pacientes, con un intervalo
de edad de 43–90 años (Tabla 3).
De los pacientes remitidos se ha confirmado el diagnostico de Insuficiencia cardiaca
en 36 pacientes y las causas quedan reflejadas en la Figura 3.
3. Resultados UAR en el periodo de junio y julio 2011: Se han valorado un total de
20 pacientes, con un intervalo de edad de 25 a 88 años, de los cuales 9 pacientes
tenían más 80 años. El motivo de la derivación se describe en la Tabla 4.
Los resultados de la resolución del proceso que ha motivado la consulta y el tipo
de derivación se muestran en la Figura 4.
4. Resultados de la consultoría no presencial: Se han valorado en un periodo de 3
meses un total de 34 consultas que se han solucionado en 32 casos. Sólo en dos de
las consultas ha sido necesaria la valoración presencial (por la UAR o en consulta
ordinaria).
Discusión
Hasta el año 2005 en nuestro entorno asistencial la relación entre los diferentes
niveles era testimonial. A pesar de que ha habido iniciativas importantes desde la
AP- Atención Especializada, con buena acogida por ésta última, no ha llegado a cristalizar
una relación directa interniveles. A partir de que la AC es asumida por nuestro hospital,
se ponen en marcha toda una serie de intervenciones, con la finalidad de consensuar
con la primaria, así como con el tercer nivel asistencial, las rutas y los criterios
de actuación según las guías de práctica clínica, para dar continuidad asistencial
al paciente independientemente del nivel asistencial donde sea tratado.
Conclusiones
El consenso entre los diferentes niveles asistenciales implicados en el proceso, desde
una visión de cliente proveedor (AP-Hospital), es imprescindible para determinar en
base a la necesidad asistencial y el principio de subsidiaridad quien hace que y donde
se realiza.
Con la puesta en marcha de las nuevas medidas en la atención integral del paciente,
se espera dar respuesta al proceso que motiva la consulta en la mayor parte de los
casos de forma breve y eficaz. Nuestra visión es disponer de un servicio de cardiología
capaz de adecuar sus respuestas asistenciales a la necesidad asistencial del proceso
solicitado desde el nivel asistencial cliente.
Related collections
Most cited references5
- Record: found
- Abstract: found
- Article: not found
[Coordination among healthcare levels: systematization of tools and measures].
- Record: found
- Abstract: found
- Article: not found
Geographically-decentralized planning and management in health care: some informational issues and their implications for efficiency.
Greg J. Bishop-Hurley, Stephen J. Eyles, S Birch (1995)
- Record: found
- Abstract: found
- Article: not found