- Record: found
- Abstract: found
- Article: found
Claims‐Based Algorithms for Identifying Patients With Pulmonary Hypertension: A Comparison of Decision Rules and Machine‐Learning Approaches
Read this article at
Abstract
Background
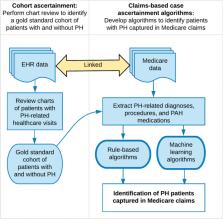
Real‐world healthcare data are an important resource for epidemiologic research. However, accurate identification of patient cohorts—a crucial first step underpinning the validity of research results—remains a challenge. We developed and evaluated claims‐based case ascertainment algorithms for pulmonary hypertension (PH), comparing conventional decision rules with state‐of‐the‐art machine‐learning approaches.
Methods and Results
We analyzed an electronic health record‐Medicare linked database from two large academic tertiary care hospitals (years 2007–2013). Electronic health record charts were reviewed to form a gold standard cohort of patients with (n=386) and without PH (n=164). Using health encounter data captured in Medicare claims (including patients’ demographics, diagnoses, medications, and procedures), we developed and compared 2 approaches for identifying patients with PH: decision rules and machine‐learning algorithms using penalized lasso regression, random forest, and gradient boosting machine. The most optimal rule‐based algorithm—having ≥3 PH‐related healthcare encounters and having undergone right heart catheterization—attained an area under the receiver operating characteristic curve of 0.64 (sensitivity, 0.75; specificity, 0.48). All 3 machine‐learning algorithms outperformed the most optimal rule‐based algorithm ( P<0.001). A model derived from the random forest algorithm achieved an area under the receiver operating characteristic curve of 0.88 (sensitivity, 0.87; specificity, 0.70), and gradient boosting machine achieved comparable results (area under the receiver operating characteristic curve, 0.85; sensitivity, 0.87; specificity, 0.70). Penalized lasso regression achieved an area under the receiver operating characteristic curve of 0.73 (sensitivity, 0.70; specificity, 0.68).
Conclusions
Research‐grade case identification algorithms for PH can be derived and rigorously validated using machine‐learning algorithms. Simple decision rules commonly applied in published literature performed poorly; more complex rule‐based algorithms may potentially address the limitation of this approach. PH research using claims data would be considerably strengthened through the use of validated algorithms for cohort ascertainment.
Related collections
Most cited references23

- Record: found
- Abstract: found
- Article: found
Haemodynamic definitions and updated clinical classification of pulmonary hypertension
- Record: found
- Abstract: found
- Article: not found
A method of comparing the areas under receiver operating characteristic curves derived from the same cases.
- Record: found
- Abstract: not found
- Article: not found