- Record: found
- Abstract: found
- Article: found
Implications of False Negative and False Positive Diagnosis in Lymph Node Staging of NSCLC by Means of 18F-FDG PET/CT
Read this article at
Abstract
Background
Integrated 18F-fluorodeoxyglucose positron emission tomography/computed tomography ( 18F-FDG PET/CT) is widely performed in hilar and mediastinal lymph node (HMLN) staging of non-small cell lung cancer (NSCLC). However, the diagnostic efficiency of PET/CT remains controversial. This retrospective study is to evaluate the accuracy of PET/CT and the characteristics of false negatives and false positives to improve specificity and sensitivity.
Methods
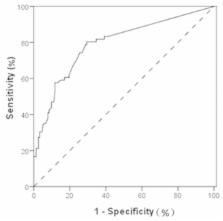
219 NSCLC patients with systematic lymph node dissection or sampling underwent preoperative PET/CT scan. Nodal uptake with a maximum standardized uptake value (SUVmax) >2.5 was interpreted as PET/CT positive. The results of PET/CT were compared with the histopathological findings. The receiver operating characteristic (ROC) curve was generated to determine the diagnostic efficiency of PET/CT. Univariate and multivariate analysis were conducted to detect risk factors of false negatives and false positives.
Results
The sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and accuracy of PET/ CT in detecting HMLN metastases were 74.2% (49/66), 73.2% (112/153), 54.4% (49/90), 86.8% (112/129), and 73.5% (161/219). The ROC curve had an area under curve (AUC) of 0.791 (95% CI 0.723-0.860). The incidence of false negative HMLN metastases was 13.2% (17 of 129 patients). Factors that are significantly associated with false negatives are: concurrent lung disease or diabetes (p<0.001), non-adenocarcinoma (p<0.001), and SUVmax of primary tumor >4.0 (p=0.009). Postoperatively, 45.5% (41/90) patients were confirmed as false positive cases. The univariate analysis indicated age > 65 years old (p=0.009), well differentiation (p=0.002), and SUVmax of primary tumor ≦4.0 (p=0.007) as risk factors for false positive uptake.
Related collections
Most cited references16
- Record: found
- Abstract: found
- Article: not found
Clinical applications of PET in oncology.
- Record: found
- Abstract: found
- Article: not found
Patterns of disease recurrence after stereotactic ablative radiotherapy for early stage non-small-cell lung cancer: a retrospective analysis.
- Record: found
- Abstract: found
- Article: not found