- Record: found
- Abstract: found
- Article: found
Assessment of Mobile Health Apps Using Built-In Smartphone Sensors for Diagnosis and Treatment: Systematic Survey of Apps Listed in International Curated Health App Libraries
Abstract
Background
More than a million health and well-being apps are available from the Apple and Google app stores. Some apps use built-in mobile phone sensors to generate health data. Clinicians and patients can find information regarding safe and effective mobile health (mHealth) apps in third party–curated mHealth app libraries.
Objective
These independent Web-based repositories guide app selection from trusted lists, but do they offer apps using ubiquitous, low-cost smartphone sensors to improve health? This study aimed to identify the types of built-in mobile phone sensors used in apps listed on curated health app libraries, the range of health conditions these apps address, and the cross-platform availability of the apps.
Methods
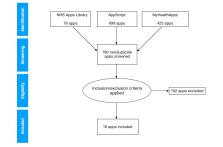
This systematic survey reviewed three such repositories (National Health Service Apps Library, AppScript, and MyHealthApps), assessing the availability of apps using built-in mobile phone sensors for the diagnosis or treatment of health conditions.
Results
A total of 18 such apps were identified and included in this survey, representing 1.1% (8/699) to 3% (2/76) of all apps offered by the respective libraries examined. About one-third (7/18, 39%) of the identified apps offered cross-platform Apple and Android versions, with a further 50% (9/18) only dedicated to Apple and 11% (2/18) to Android. About one-fourth (4/18, 22%) of the identified apps offered dedicated diagnostic functions, with a majority featuring therapeutic (9/18, 50%) or combined functionality (5/18, 28%). Cameras, touch screens, and microphones were the most frequently used built-in sensors. Health concerns addressed by these apps included respiratory, dermatological, neurological, and anxiety conditions.
Conclusions
Diligent mHealth app library curation, medical device regulation constraints, and cross-platform differences in mobile phone sensor architectures may all contribute to the observed limited availability of mHealth apps using built-in phone sensors in curated mHealth app libraries. However, more efforts are needed to increase the number of such apps on curated lists, as they offer easily accessible low-cost options to assist people in managing clinical conditions.
Related collections
Most cited references40
- Record: found
- Abstract: found
- Article: not found
Systematic review of smartphone-based passive sensing for health and wellbeing
- Record: found
- Abstract: found
- Article: not found
Consumer Mobile Health Apps: Current State, Barriers, and Future Directions.

- Record: found
- Abstract: found
- Article: found