- Record: found
- Abstract: found
- Article: found
Overall survival and clinical characteristics of pancreatic cancer in BRCA mutation carriers
Read this article at
Abstract
Background:
The BRCA1/2 proteins are involved in regulation of cellular proliferation by DNA damage repair via homologous recombination. Therefore, BRCA1/2 mutation carriers with pancreatic cancer may have distinct biologic outcomes.
Methods:
Patients with BRCA1/2-associated pancreatic ductal adenocarcinoma (PDAC) diagnosed between January 1994 and December 2012 were identified from databases at three participating institutions. Clinical data were collected. Disease-free survival and overall survival (OS) were analysed.
Results:
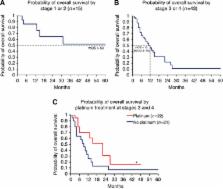
Overall, 71 patients with PDAC and BRCA1 ( n=21), BRCA2 ( n=49) or both ( n=1) mutations were identified. Mean age at diagnosis was 60.3 years (range 33–83), 81.7% ( n=58) had any family history of malignancy; 30% ( n=21) underwent primary resection. Out of 71 participants, 12 received experimental therapy; one patient had missing data, these 13 cases were excluded from OS analysis. Median OS for 58 patients was 14 months (95% CI 10–23 months). Median OS for patients with stage 1/2 disease has not been reached with 52% still alive at 60 months. Median OS for stage 3/4 was 12 months (95% CI 6–15). Superior OS was observed for patients with stage 3/4 treated with platinum vs those treated with non-platinum chemotherapies (22 vs 9 months; P=0.039).
Related collections
Most cited references31
- Record: found
- Abstract: found
- Article: not found