- Record: found
- Abstract: found
- Article: found
Gelatin Nanoparticles-HPMC Hybrid System for Effective Ocular Topical Administration of Antihypertensive Agents
Read this article at
Abstract
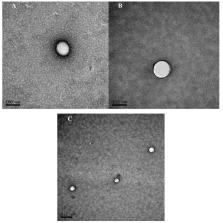
The increment in ocular drug bioavailability after topical administration is one of the main challenges in pharmaceutical technology. For several years, different strategies based on nanotechnology, hydrogels or implants have been evaluated. Nowadays, the tolerance of ophthalmic preparations has become a critical issue and it is essential to the use of well tolerated excipients. In the present work, we have explored the potential of gelatin nanoparticles (GNPs) loaded with timolol maleate (TM), a beta-adrenergic blocker widely used in the clinic for glaucoma treatment and a hybrid system of TM-GNPs included in a hydroxypropyl methylcellulose (HPMC) viscous solution. The TM- loaded nanoparticles (mean particle size of 193 ± 20 nm and drug loading of 0.291 ± 0.019 mg TM/mg GNPs) were well tolerated both in vitro (human corneal cells) and in vivo. The in vivo efficacy studies performed in normotensive rabbits demonstrated that these gelatin nanoparticles were able to achieve the same hypotensive effect as a marketed formulation (0.5% TM) containing a 5-fold lower concentration of the drug. When comparing commercial and TM-GNPs formulations with the same TM dose, nanoparticles generated an increased efficacy with a significant ( p < 0.05) reduction of intraocular pressure (IOP) (from 21% to 30%) and an augmentation of 1.7-fold in the area under the curve (AUC) (0–12h). On the other hand, the combination of timolol-loaded nanoparticles (TM 0.1%) and the viscous polymer HPMC 0.3%, statistically improved the IOP reduction up to 30% (4.65 mmHg) accompanied by a faster time of maximum effect (t max = 1 h). Furthermore, the hypotensive effect was extended for four additional hours, reaching a pharmacological activity that lasted 12 h after a single instillation of this combination, and leading to an AUC (0–12h) 2.5-fold higher than the one observed for the marketed formulation. According to the data presented in this work, the use of hybrid systems that combine well tolerated gelatin nanoparticles and a viscous agent could be a promising alternative in the management of high intraocular pressure in glaucoma.
Related collections
Most cited references77
- Record: found
- Abstract: found
- Article: not found
Preservatives in eyedrops: the good, the bad and the ugly.
- Record: found
- Abstract: found
- Article: not found
Analysis of Cell Viability by the MTT Assay
- Record: found
- Abstract: found
- Article: not found