- Record: found
- Abstract: found
- Article: found
Efficacy and safety at 6 months of the XEN implant for the management of open angle glaucoma
Read this article at
Abstract
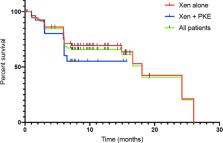
The purpose of this study is to evaluate the efficacy and complications of the XEN implant as a solo procedure or in association with cataract surgery in patients with open angle glaucoma (OAG). All patients who received a XEN implant between June 2017 and June 2018 were included in the study. The primary and secondary outcomes were: the reduction of the intraocular pressure (IOP) at 6 months postoperatively, the decrease of the glaucoma medications 6 months after surgery, the clinical success rate (eyes (%) achieving ≥20% IOP reduction on the same or fewer medications without secondary surgical intervention), the frequency and type of postoperative interventions as well as the complication rate. We included one hundred and seven eyes from 97 patients with primary OAG (79%), or secondary OAG (21%). Seventy-seven patients (72%) received a standalone XEN implantation and 30 (28%) underwent XEN implantation combined with phacoemusification. The IOP decreased from 20.4 mm Hg ± 6.4 preoperatively to 15.4 mm Hg ± 5.3 six months after the surgery, which represented a reduction of 24.5% ( P = 1.4.10 −7). It was associated with a lowering of glaucoma medications from 2.8 ± 1.0 preoperatively to 0.6 ± 1.0 six months postoperatively ( P = 3.6.10 −34). The clinical success rate was 67.2% six months after the surgery. The most frequent complications were: IOP spikes >30 mmHg (16.8%), improper position or angled drain (14.0%) and transient minimal hyphema (<1 week) (11.2%). During the follow-up, the needling was required in 34.6% of cases and a total of 10 eyes (9.4%) required a new glaucoma surgery. To conclude XEN implantation appears to be an effective short- and mid-term surgical technique to control IOP in OAG with a low risk of complication. However postoperative maneuvers were frequently required to maintain efficiency.
Related collections
Most cited references16
- Record: found
- Abstract: found
- Article: not found
The Advanced Glaucoma Intervention Study (AGIS): 7. The relationship between control of intraocular pressure and visual field deterioration.The AGIS Investigators.
- Record: found
- Abstract: found
- Article: found
Glaucoma is second leading cause of blindness globally

- Record: found
- Abstract: found
- Article: found