- Record: found
- Abstract: found
- Article: found
Prospective One Year Follow Up of HIV Infected Women Screened for Cervical Cancer Using Visual Inspection with Acetic Acid, Cytology and Human Papillomavirus Testing in Johannesburg South Africa
Read this article at
Abstract
Background
Cervical cancer is the most common cancer in Sub-Saharan Africa. There are little of HIV-infected women one-year after screening using visual inspection with acetic acid (VIA), HPV or cytology in sub-Saharan Africa.
Methods
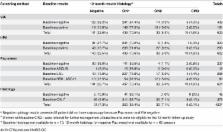
HIV-infected women in Johannesburg South Africa were screened one year later by Pap smear, VIA and human papillomavirus (HPV) testing. Women qualified for the 12 month follow-up visit if they had a negative or cervical intra-epithelial neoplasia (CIN) 1 results at the baseline visit. Modified Poisson regression was used to analyse associations between patient baseline characteristics and progression.
Results
A total of 688 of 1,202 enrolled at baseline study who were CIN-2+ negative and qualified for a 12 month follow-up visit. Progression to CIN-2+ was higher in women with positive VIA results (12.6%; 24/191) than those VIA-negative (4.4%; 19/432). HPV-positive women at baseline were more likely to progress to CIN-2+ (12.3%; 36/293) than those HPV-negative (2.1%; 7/329). Cytology-positive women at baseline were more likely to progress to CIN-2+ (9.6%; 37/384) than cytology-negative women (2.5%; 6/237). Approximately 10% (10.4%; 39/376) of women with CIN 1 at baseline progressed to CIN 2+. Women who were VIA or HPV positive at baseline were more likely to progress aIRR 1.85, CI 95% (1.46 to 2.36), aIRR 1.41 CI 95% (1.14 to 1.75) respectively.
Related collections
Most cited references8
- Record: found
- Abstract: found
- Article: not found
Human papillomavirus-associated cancers in patients with human immunodeficiency virus infection and acquired immunodeficiency syndrome.
- Record: found
- Abstract: found
- Article: not found
Risk of human papillomavirus-associated cancers among persons with AIDS.
- Record: found
- Abstract: found
- Article: not found