- Record: found
- Abstract: found
- Article: not found
Cognitive impairments four months after COVID-19 hospital discharge: pattern, severity and association with illness variables
Read this article at
Abstract
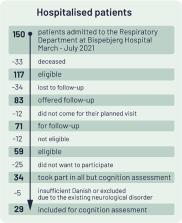
The ongoing Coronavirus Disease 2019 (COVID-19) pandemic has affected more than 100 million people and clinics are being established for diagnosing and treating lingering symptoms, so called long-COVID. A key concern are neurological and long-term cognitive complications. At the same time, the prevalence and nature of the cognitive sequalae of COVID-19 are unclear. The present study aimed to investigate the frequency, pattern and severity of cognitive impairments 3-4 months after COVID-19 hospital discharge, their relation to subjective cognitive complaints, quality of life and illness variables. We recruited patients at their follow-up visit at the respiratory outpatient clinic, Copenhagen University Hospital, Bispebjerg, approximately four months after hospitalisation with COVID-19. Patients underwent pulmonary, functional and cognitive assessments. Twenty-nine patients were included. The percentage of patients with clinically significant cognitive impairment ranged from 59-65% depending on the applied cut-off for clinical relevance of cognitive impairment, with verbal learning and executive functions being most affected. Objective cognitive impairment scaled with subjective cognitive complaints, lower work function and poorer quality of life. Cognitive impairments were associated with d-dimer levels during acute illness and residual pulmonary dysfunction. In conclusion, these findings provide new evidence for frequent cognitive sequelae of COVID-19 and indicate an association with the severity of the lung affection and potentially restricted cerebral oxygen delivery. Further, the associations with quality of life and functioning call for systematic cognitive screening of patients after recovery from severe COVID-19 illness and implementation of targeted treatments for patients with persistent cognitive impairments.
Related collections
Most cited references47
- Record: found
- Abstract: found
- Article: not found
Neurologic Manifestations of Hospitalized Patients With Coronavirus Disease 2019 in Wuhan, China
- Record: found
- Abstract: found
- Article: not found
6-month consequences of COVID-19 in patients discharged from hospital: a cohort study
- Record: found
- Abstract: found
- Article: not found
