- Record: found
- Abstract: found
- Article: found
Differential Diagnosis of Retinal Vasculitis
meeting-report
Read this article at
There is no author summary for this article yet. Authors can add summaries to their articles on ScienceOpen to make them more accessible to a non-specialist audience.
Abstract
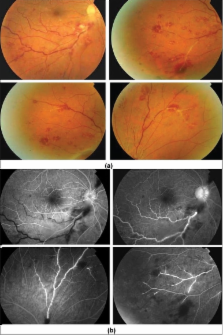
Retinal vaculitis is a sight-threatening inflammatory eye condition that involves the retinal vessels. Detection of retinal vasculitis is made clinically, and confirmed with the help of fundus fluorescein angiography. Active vascular disease is characterized by exudates around retinal vessels resulting in white sheathing or cuffing of the affected vessels. In this review, a practical approach to the diagnosis of retinal vasculitis is discussed based on ophthalmoscopic and fundus fluorescein angiographic findings.
Related collections
Most cited references100
- Record: found
- Abstract: not found
- Article: not found
Standard diagnostic criteria for the acute retinal necrosis syndrome. Executive Committee of the American Uveitis Society.
Daniel G Holland (1994)
- Record: found
- Abstract: found
- Article: not found
Viral causes of the acute retinal necrosis syndrome.
Jyotsom B Ganatra, Diane J. Chandler, Carmen Santos … (2000)
- Record: found
- Abstract: found
- Article: not found
Ocular complications of Rift Valley fever outbreak in Saudi Arabia.
Ali Hazmi, Lubna N Ahmed, Mohammed Al Dosari … (2005)