- Record: found
- Abstract: found
- Article: found
Improved Diagnostics Help to Identify Clinical Features and Biomarkers That Predict Mycoplasma pneumoniae Community-acquired Pneumonia in Children
Read this article at
Abstract
Background
There are no reliable signs or symptoms that differentiate Mycoplasma pneumoniae ( Mp) infection in community-acquired pneumonia (CAP) from other etiologies. Additionally, current diagnostic tests do not reliably distinguish between Mp infection and carriage. We previously determined that the measurement of Mp-specific immunoglobulin M antibody-secreting cells (ASCs) by enzyme-linked immunospot assay allowed for differentiation between infection and carriage. Using this new diagnostic test, we aimed to identify clinical and laboratory features associated with Mp infection.
Methods
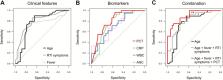
This is a prospective cohort study of children, 3–18 years of age, with CAP from 2016 to 2017. Clinical features and biomarkers were compared between Mp-positive and -negative groups by Mann-Whitney U test or Fisher exact test, as appropriate. Area under the receiver operating characteristic curve (AUC) differences and optimal thresholds were determined by using the DeLong test and Youden J statistic, respectively.
Results
Of 63 CAP patients, 29 were Mp-positive (46%). Mp positivity was statistically associated with older age (median, 8.6 vs 4.7 years), no underlying disease, family with respiratory symptoms, prior antibiotic treatment, prolonged prodromal respiratory symptoms and fever, and extrapulmonary (skin) manifestations. Lower levels of C-reactive protein, white blood cell count, absolute neutrophil count, and procalcitonin (PCT), specifically PCT <0.25 μg/L, were statistically associated with Mp infection. A combination of age >5 years (AUC = 0.77), prodromal fever and respiratory symptoms >6 days (AUC = 0.79), and PCT <0.25 μg/L (AUC = 0.81) improved diagnostic performance (AUC = 0.90) ( P = .05).
Abstract
Community-acquired pneumonia (CAP) caused by Mycoplasma pneumoniae ( Mp) is difficult to diagnose. A combination of clinical features and biomarkers may aid physicians in identifying patients at high risk for Mp CAP.
Related collections
Most cited references40
- Record: found
- Abstract: found
- Article: not found
Community-acquired pneumonia requiring hospitalization among U.S. children.
- Record: found
- Abstract: found
- Article: found
Causes of severe pneumonia requiring hospital admission in children without HIV infection from Africa and Asia: the PERCH multi-country case-control study
- Record: found
- Abstract: found
- Article: not found