- Record: found
- Abstract: found
- Article: found
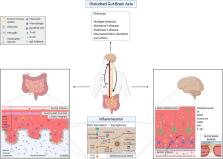
The Gut-Brain Axis: How Microbiota and Host Inflammasome Influence Brain Physiology and Pathology
Read this article at
Abstract
The human microbiota has a fundamental role in host physiology and pathology. Gut microbial alteration, also known as dysbiosis, is a condition associated not only with gastrointestinal disorders but also with diseases affecting other distal organs. Recently it became evident that the intestinal bacteria can affect the central nervous system (CNS) physiology and inflammation. The nervous system and the gastrointestinal tract are communicating through a bidirectional network of signaling pathways called the gut-brain axis, which consists of multiple connections, including the vagus nerve, the immune system, and bacterial metabolites and products. During dysbiosis, these pathways are dysregulated and associated with altered permeability of the blood-brain barrier (BBB) and neuroinflammation. However, numerous mechanisms behind the impact of the gut microbiota in neuro-development and -pathogenesis remain poorly understood. There are several immune pathways involved in CNS homeostasis and inflammation. Among those, the inflammasome pathway has been linked to neuroinflammatory conditions such as multiple sclerosis, Alzheimer’s and Parkinson’s diseases, but also anxiety and depressive-like disorders. The inflammasome complex assembles upon cell activation due to exposure to microbes, danger signals, or stress and lead to the production of pro-inflammatory cytokines (interleukin-1β and interleukin-18) and to pyroptosis. Evidences suggest that there is a reciprocal influence of microbiota and inflammasome activation in the brain. However, how this influence is precisely working is yet to be discovered. Herein, we discuss the status of the knowledge and the open questions in the field focusing on the function of intestinal microbial metabolites or products on CNS cells during healthy and inflammatory conditions, such as multiple sclerosis, Alzheimer’s and Parkinson’s diseases, and also neuropsychiatric disorders. In particular, we focus on the innate inflammasome pathway as immune mechanism that can be involved in several of these conditions, upon exposure to certain microbes.
Related collections
Most cited references256

- Record: found
- Abstract: found
- Article: found
Structure, Function and Diversity of the Healthy Human Microbiome
- Record: found
- Abstract: found
- Article: not found