- Record: found
- Abstract: found
- Article: found
Differentiation of human male germ cells from Wharton's jelly-derived mesenchymal stem cells
Read this article at
Abstract
Objective
Recapitulation of the spermatogenesis process in vitro is a tool for studying the biology of germ cells, and may lead to promising therapeutic strategies in the future. In this study, we attempted to transdifferentiate Wharton's jelly-derived mesenchymal stem cells (WJ-MSCs) into male germ cells using all- trans retinoic acid and Sertoli cell-conditioned medium.
Methods
Human WJ-MSCs were propagated by the explant culture method, and cells at the second passage were induced with differentiation medium containing all- trans retinoic acid for 2 weeks. Putative germ cells were cultured with Sertoli cell-conditioned medium at 36℃ for 3 more weeks.
Results
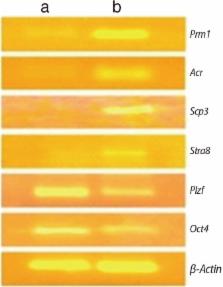
The gene expression profile was consistent with the stage-specific development of germ cells. The expression of Oct4 and Plzf (early germ cell markers) was diminished, while Stra8 (a premeiotic marker), Scp3 (a meiotic marker), and Acr and Prm1 (postmeiotic markers) were upregulated during the induction period. In morphological studies, approximately 5% of the cells were secondary spermatocytes that had completed two stages of acrosome formation (the Golgi phase and the cap phase). A few spermatid-like cells that had undergone the initial stage of tail formation were also noted.
Related collections
Most cited references36
- Record: found
- Abstract: found
- Article: not found
Spermatogenic cells of the prepuberal mouse: isolation and morphological characterization
- Record: found
- Abstract: found
- Article: not found
The central role of Sertoli cells in spermatogenesis.
- Record: found
- Abstract: found
- Article: not found