- Record: found
- Abstract: found
- Article: found
Predictive Model of the Risk of In-Hospital Mortality in Colorectal Cancer Surgery, Based on the Minimum Basic Data Set
Read this article at
Abstract
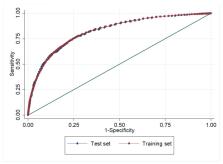
Background: Various models have been proposed to predict mortality rates for hospital patients undergoing colorectal cancer surgery. However, none have been developed in Spain using clinical administrative databases and none are based exclusively on the variables available upon admission. Our study aim is to detect factors associated with in-hospital mortality in patients undergoing surgery for colorectal cancer and, on this basis, to generate a predictive mortality score. Methods: A population cohort for analysis was obtained as all hospital admissions for colorectal cancer during the period 2008–2014, according to the Spanish Minimum Basic Data Set. The main measure was actual and expected mortality after the application of the considered mathematical model. A logistic regression model and a mortality score were created, and internal validation was performed. Results: 115,841 hospitalization episodes were studied. Of these, 80% were included in the training set. The variables associated with in-hospital mortality were age (OR: 1.06, 95%CI: 1.05–1.06), urgent admission (OR: 4.68, 95% CI: 4.36–5.02), pulmonary disease (OR: 1.43, 95%CI: 1.28–1.60), stroke (OR: 1.87, 95%CI: 1.53–2.29) and renal insufficiency (OR: 7.26, 95%CI: 6.65–7.94). The level of discrimination (area under the curve) was 0.83. Conclusions: This mortality model is the first to be based on administrative clinical databases and hospitalization episodes. The model achieves a moderate–high level of discrimination.
Related collections
Most cited references25
- Record: found
- Abstract: found
- Article: not found
POSSUM: a scoring system for surgical audit.
- Record: found
- Abstract: found
- Article: not found
Postoperative mortality and morbidity in French patients undergoing colorectal surgery: results of a prospective multicenter study.
- Record: found
- Abstract: found
- Article: not found