- Record: found
- Abstract: found
- Article: found
Human Papillomavirus Vaccine Awareness and Acceptability for Primary Prevention of Cervical Cancer in Pakistan: A Cross-Sectional Study
Read this article at
Abstract
Background:
Human papillomavirus (HPV) vaccine is the most effective option for primary prevention HPV, a well-known cause of cervical cancer. The objective of the study was to assess awareness of HPV, the acceptability of its vaccine and factors associated with the acceptability among the adult population in Pakistan.
Materials and Methods:
A cross-sectional survey was conducted among adult population of Pakistan from January 2022 and March 2022. Due to the ongoing COVID-19 pandemic, instead of face-to-face interviews, a self-administered questionnaire was developed and distributed through Google Forms. The questionnaire was available in both English and Urdu languages to cater to a diverse population.
Results:
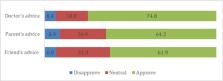
Overall, 313 (65.2 %) study participants had heard about HPV infection, while 297 (61.9%) knew HPV as the cause of genital warts and 256 (53.3 %) knew that HPV can cause any type of cancer, with a higher percentage of awareness among those who were in any health care setting compared to those who were in a non-healthcare setting. Regarding the acceptability to get HPV vaccine, 320 (66.7%) of the study participants were willing to get vaccinated, while only 15(3.1%) of the study population had previously received HPV vaccine. The most important factors associated with HPV vaccine acceptability were younger age of 18-25 years (Prevalence Ratio (PR) =1.60, 95% Confidence Interval (CI) =1.11, 2.32), and 26-35 years (PR= 1.65, 95% CI=1.09, 2.50). HPV vaccine acceptability was also associated with working in a healthcare setting due to better awareness of HPV vaccine (PR= 1.29, 95% CI=1.03, 1.62).
Conclusion:
It is important to address the knowledge gaps existing in the community about HPV vaccine acceptability and barriers against it for the successful rollout of the HPV vaccination program in Pakistan. Mass awareness campaigns about HPV, HPV vaccine, and cervical cancer are needed to increase the acceptability of HPV vaccine among public at the time of reintroducing HPV vaccine.
Related collections
Most cited references32

- Record: found
- Abstract: found
- Article: found
Impact of HPV vaccination and cervical screening on cervical cancer elimination: a comparative modelling analysis in 78 low-income and lower-middle-income countries

- Record: found
- Abstract: found
- Article: found