- Record: found
- Abstract: found
- Article: not found
Evidence-Based Treatment for Melasma: Expert Opinion and a Review
Read this article at
Abstract
Introduction
Melasma is one of the most common pigmentary disorders seen by dermatologists and often occurs among women with darker complexion (Fitzpatrick skin type IV–VI). Even though melasma is a widely recognized cause of significant cosmetic disfigurement worldwide and in India, there is a lack of systematic and clinically usable treatment algorithms and guidelines for melasma management. The present article outlines the epidemiology of melasma, reviews the various treatment options along with their mode of action, underscores the diagnostic dilemmas and quantification of illness, and weighs the evidence of currently available therapies.
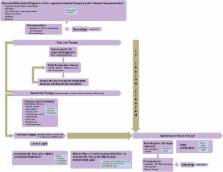
Methods
A panel of eminent dermatologists was created and their expert opinion was sought to address lacunae in information to arrive at a working algorithm for optimizing outcome in Indian patients. A thorough literature search from recognized medical databases preceded the panel discussions. The discussions and consensus from the panel discussions were drafted and refined as evidence-based treatment for melasma. The deployment of this algorithm is expected to act as a basis for guiding and refining therapy in the future.
Results
It is recommended that photoprotection and modified Kligman’s formula can be used as a first-line therapy for up to 12 weeks. In most patients, maintenance therapy will be necessary with non-hydroquinone (HQ) products or fixed triple combination intermittently, twice a week or less often. Concomitant camouflage should be offered to the patient at any stage during therapy. Monthly follow-ups are recommended to assess the compliance, tolerance, and efficacy of therapy.
Related collections
Most cited references109
- Record: found
- Abstract: found
- Article: not found
Hypopigmenting agents: an updated review on biological, chemical and clinical aspects.
- Record: found
- Abstract: found
- Article: not found
Chemical and instrumental approaches to treat hyperpigmentation.
- Record: found
- Abstract: found
- Article: not found
