- Record: found
- Abstract: found
- Article: found
Mixed storm in SARS‐CoV‐2 infection: A narrative review and new term in the Covid‐19 era
Read this article at
Abstract
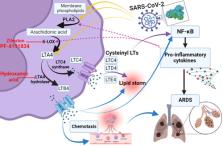
Coronavirus disease 2019 (Covid‐19) is caused by a novel severe acute respiratory syndrome coronavirus virus type 2 (SARS‐CoV‐2) leading to the global pandemic worldwide. Systemic complications in Covid‐19 are mainly related to the direct SARS‐CoV‐2 cytopathic effects, associated hyperinflammation, hypercytokinemia, and the development of cytokine storm (CS). As well, Covid‐19 complications are developed due to the propagation of oxidative and thrombotic events which may progress to a severe state called oxidative storm and thrombotic storm (TS), respectively. In addition, inflammatory and lipid storms are also developed in Covid‐19 due to the activation of inflammatory cells and the release of bioactive lipids correspondingly. Therefore, the present narrative review aimed to elucidate the interrelated relationship between different storm types in Covid‐19 and the development of the mixed storm (MS). In conclusion, SARS‐CoV‐2 infection induces various storm types including CS, inflammatory storm, lipid storm, TS and oxidative storm. These storms are not developing alone since there is a close relationship between them. Therefore, the MS seems to be more appropriate to be related to severe Covid‐19 than CS, since it develops in Covid‐19 due to the intricate interface between reactive oxygen species, proinflammatory cytokines, complement activation, coagulation disorders, and activated inflammatory signaling pathway.
Abstract
SARS‐CoV‐2 infection induces various storm types including cytokine storm (CS), inflammatory storm, lipid storm, thrombotic storm (TS), and oxidative storm. These storms are not developing alone since there is a close relationship between them. Therefore, the mixed storm seems to be more appropriate to be related to severe Covid‐19 than CS, since it develops in Covid‐19 due to the intricate interface between reactive oxygen species, proinflammatory cytokines, complement activation, coagulation disorders, and activated inflammatory signaling pathway
Related collections
Most cited references193
- Record: found
- Abstract: found
- Article: not found
Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China
- Record: found
- Abstract: found
- Article: found
COVID-19: consider cytokine storm syndromes and immunosuppression
- Record: found
- Abstract: found
- Article: not found
