- Record: found
- Abstract: found
- Article: found
Hypercoagulability and Mortality of Patients with Stroke and Active Cancer: The OASIS-CANCER Study
Read this article at
Abstract
Background and Purpose
Patients with active cancer are at an increased risk for stroke. Hypercoagulability plays an important role in cancer-related stroke. We aimed to test whether 1) hypercoagulability is a predictor of survival, and 2) correction of the hypercoagulable state leads to better survival in patients with stroke and active cancer.
Methods
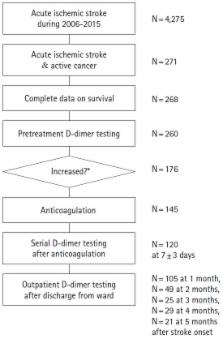
We recruited consecutive patients with acute ischemic stroke and active systemic cancer between January 2006 and July 2015. Hypercoagulability was assessed using plasma D-dimer levels before and after 7 days of anticoagulation treatment. The study outcomes included overall and 1-year survival. Plasma D-dimer levels before and after treatment were tested in univariate and multivariate Cox regression models. We controlled for systemic metastasis, stroke mechanism, age, stroke severity, primary cancer type, histology, and atrial fibrillation using the forward stepwise method.
Results
A total of 268 patients were included in the analysis. Patients with high (3rd–4th quartiles) pre-treatment plasma D-dimer levels showed decreased overall and 1-year survival (adjusted HR, 2.19 [95% CI, 1.46–3.31] and 2.70 [1.68–4.35], respectively). After anticoagulation treatment, post-treatment D-dimer level was significantly reduced and independently associated with poor 1-year survival (adjusted HR, 1.03 [95% CI, 1.01–1.05] per 1 μg/mL increase, P=0.015). The successful correction of hypercoagulability was a protective factor for 1-year survival (adjusted HR 0.26 [CI 0.10–0.68], P=0.006).
Related collections
Most cited references31
- Record: found
- Abstract: found
- Article: not found
Membrane-derived microvesicles: important and underappreciated mediators of cell-to-cell communication.
- Record: found
- Abstract: found
- Article: not found
Low-molecular-weight heparin versus a coumarin for the prevention of recurrent venous thromboembolism in patients with cancer.
- Record: found
- Abstract: found
- Article: not found