- Record: found
- Abstract: found
- Article: found
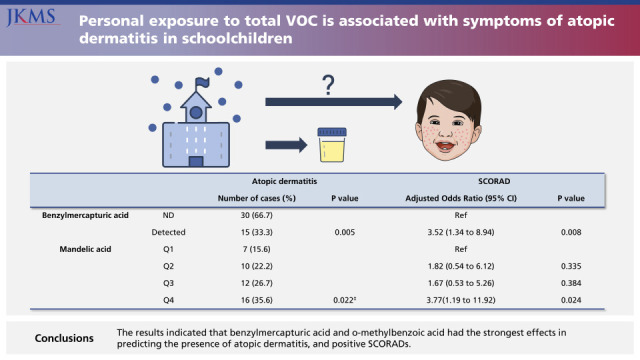
Personal Exposure to Total VOC is Associated With Symptoms of Atopic Dermatitis in Schoolchildren

Read this article at
Abstract
Background
The urinary levels of volatile organic compound (VOC) metabolites provide individual exposure levels compared to data obtained by measuring these compounds in ambient air. We aimed to investigate the association between personal urinary concentrations of VOC metabolites and symptoms of atopic dermatitis in schoolchildren.
Methods
Nine urinary VOC metabolites were analyzed from urine samples of 149 children. Diagnosis of atopic dermatitis was determined using standardized questionnaires. Pediatricians visited the schools and rated the severity of symptoms using the SCORing Atopic Dermatitis (SCORAD) in all children.
Results
Forty-five children (30.2%) had atopic dermatitis based on the International Study of Asthma and Allergies in Childhood (ISAAC) results and 35 children (23.8%) had symptoms of atopic dermatitis with positive SCORAD index values (defined as SCORAD ≥ 5). Children with benzylmercapturic acid detected in personal urines were associated with presence of atopic dermatitis and positive SCORAD index values. Children in the highest quartile of mandelic acid concentration were associated with presence of atopic dermatitis and positive SCORAD results.
Graphical Abstract
Related collections
Most cited references32
- Record: found
- Abstract: found
- Article: not found
The role of air pollutants in atopic dermatitis.
- Record: found
- Abstract: found
- Article: not found
Long-term exposure to close-proximity air pollution and asthma and allergies in urban children.
- Record: found
- Abstract: not found
- Article: not found