- Record: found
- Abstract: found
- Article: found
Pregnancy in a unicornuate uterus: a case report
Read this article at
Abstract
Introduction
A unicornuate uterus accounts for 2.4 to 13% of all Müllerian anomalies. A unicornuate uterus with a non-communicating rudimentary horn may be associated with gynecological and obstetric complications such as infertility, endometriosis, hematometra, urinary tract anomalies, abortions, and preterm deliveries. It has a poor reproductive outcome and pregnancy management is still unclear.
Case presentation
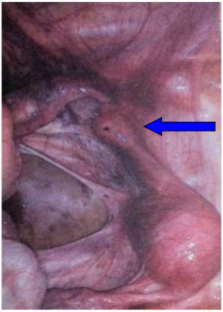
We report a case of a 26-year-old Caucasian woman presenting with a unicornuate uterus with a non-communicating rudimentary horn. The diagnosis of the anomaly was based on two-dimensional and three-dimensional sonography. The excision of her symptomatic rudimentary horn and her ipsilateral fallopian tube was performed laparoscopically. The growth of the fetus was normal. At 20 weeks’ pregnancy, her cervix started shortening and a tocolytic therapy was started. A cesarean delivery was successfully performed at 39 weeks and 4 days’ gestation.
Conclusions
Although the reproductive outcome of women with unicornuate uterus is poor, a successful pregnancy is possible. Routine excision of the rudimentary horn should be undertaken during non-pregnant state laparoscopically, and it would be necessary to screen such pregnancies for the development of intrauterine growth retardation with serial ultrasound assessments of the estimated fetal weight and the cervix length.
Related collections
Most cited references13
- Record: found
- Abstract: found
- Article: not found
Pregnancy outcomes in unicornuate uteri: a review.
- Record: found
- Abstract: found
- Article: not found
Reproductive performance of women with müllerian anomalies.
- Record: found
- Abstract: found
- Article: not found