- Record: found
- Abstract: found
- Article: found
Associations between plasma sulfur amino acids and specific fat depots in two independent cohorts: CODAM and The Maastricht Study
Read this article at
Abstract
Purpose
Sulfur amino acids (SAAs) have been associated with obesity and obesity-related metabolic diseases. We investigated whether plasma SAAs (methionine, total cysteine (tCys), total homocysteine, cystathionine and total glutathione) are related to specific fat depots.
Methods
We examined cross-sectional subsets from the CODAM cohort ( n = 470, 61.3% men, median [IQR]: 67 [61, 71] years) and The Maastricht Study (DMS; n = 371, 53.4% men, 63 [55, 68] years), enriched with (pre)diabetic individuals. SAAs were measured in fasting EDTA plasma with LC–MS/MS. Outcomes comprised BMI, skinfolds, waist circumference (WC), dual-energy X-ray absorptiometry (DXA, DMS), body composition, abdominal subcutaneous and visceral adipose tissues (CODAM: ultrasound, DMS: MRI) and liver fat (estimated, in CODAM, or MRI-derived, in DMS, liver fat percentage and fatty liver disease). Associations were examined with linear or logistic regressions adjusted for relevant confounders with z-standardized primary exposures and outcomes.
Results
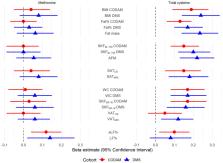
Methionine was associated with all measures of liver fat, e.g ., fatty liver disease [CODAM: OR = 1.49 (95% CI 1.19, 1.88); DMS: OR = 1.51 (1.09, 2.14)], but not with other fat depots. tCys was associated with overall obesity, e.g., BMI [CODAM: β = 0.19 (0.09, 0.28); DMS: β = 0.24 (0.14, 0.34)]; peripheral adiposity, e.g., biceps and triceps skinfolds [CODAM: β = 0.15 (0.08, 0.23); DMS: β = 0.20 (0.12, 0.29)]; and central adiposity, e.g., WC [CODAM: β = 0.16 (0.08, 0.25); DMS: β = 0.17 (0.08, 0.27)]. Associations of tCys with VAT and liver fat were inconsistent. Other SAAs were not associated with body fat.
Related collections
Most cited references77
- Record: found
- Abstract: found
- Article: not found
Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: diagnosis and classification of diabetes mellitus provisional report of a WHO consultation.
- Record: found
- Abstract: found
- Article: not found
Abdominal visceral and subcutaneous adipose tissue compartments: association with metabolic risk factors in the Framingham Heart Study.
- Record: found
- Abstract: found
- Article: not found