- Record: found
- Abstract: found
- Article: found
Acute Stroke Care in the With-COVID-19 Era: Experience at a Comprehensive Stroke Center in Japan
Read this article at
Abstract
Introduction: The pandemic of coronavirus disease 2019 (COVID-19) has had a significant impact on stroke healthcare, including the prehospital care system and in-hospital workflow. Japan experienced the outbreak of COVID-19, and the State of Emergency was declared during April 2020 and May 2020. The aim of the present study was to clarify the effect of the COVID-19 pandemic on a comprehensive stroke center in Japan.
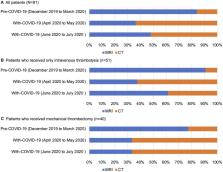
Methods: We retrospectively reviewed consecutive patients with acute ischemic stroke admitted in our institute between December 2019 and July 2020. The patients who underwent reperfusion therapy (intravenous thrombolysis and/or mechanical thrombectomy) were divided into the pre-COVID-19 period (December 2019 to March 2020) and the With-COVID-19 period (April 2020 to July 2020). Study outcomes were the number of stroke admissions in our institute, workflow time metrics, the frequency of modified Rankin Scale score 0–2 at discharge, and brain imaging modalities before reperfusion therapy in patients who underwent reperfusion therapy.
Results: In our institute, the number of stroke admissions decreased during the State of Emergency and then increased after the lifting of the State of Emergency. Among patients who underwent reperfusion therapy (median age, 77 years; female 27%; median baseline National Institutes of Health Stroke Scale score, 10), times from hospital arrival to imaging [25 (21–33) min vs. 30 (25–38) min, P = 0.03] and to thrombolysis [38 (31–52) min vs. 51 (37–64) min, P = 0.03] were prolonged compared with the pre-COVID-19 period. There was no significant difference in the frequency of modified Rankin Scale score 0–2 at discharge between the two periods (32 vs. 45%, P = 0.21). The proportion of computed tomography vs. magnetic resonance imaging as an emergency brain imaging tool before reperfusion therapy changed, with computed tomography having become predominant in the With-COVID-19 period.
Conclusions: In our institute, the number of stroke admissions, workflow time metrics, and imaging modalities for reperfusion therapy were affected by the COVID-19 pandemic.
Related collections
Most cited references20
- Record: found
- Abstract: found
- Article: not found
Neurologic Manifestations of Hospitalized Patients With Coronavirus Disease 2019 in Wuhan, China
- Record: found
- Abstract: found
- Article: not found
Large-Vessel Stroke as a Presenting Feature of Covid-19 in the Young
- Record: found
- Abstract: found
- Article: not found