- Record: found
- Abstract: found
- Article: found
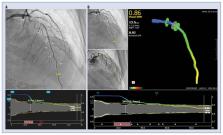
Agreement between Murray law-based quantitative flow ratio (μQFR) and three-dimensional quantitative flow ratio (3D-QFR) in non-selected angiographic stenosis: A multicenter study
Read this article at
Abstract
Background
The agreement between single-projection Murray-based quantitative flow ratio ( μQFR) and conventional three-dimensional quantitative flow ratio (3D-QFR) has not been reported hitherto.
Methods
Patients from a multinational database were randomly selected for the study of agreement, according to sample size calculation. Both conventional 3D-QFR and μQFR were analyzed for all available arteries at a central corelab by independent analysts, blinded to each other’s results.
Results
Ninety-eight coronary arteries from 35 patients were finally analyzed. Median 3D-QFR was 0.82 (interquartile range 0.78–0.87). The intraclass correlation coefficient for the absolute agreement between 3D-QFR and μQFR was 0.996 (95% confidence interval [CI]: 0.993–0.997); Lin’s coefficient 0.996 (95% CI: 0.993–0.997), without constant or proportional bias (intercept = 0 and slope = 1 in orthogonal regression). As dichotomous variable, there was absolute agreement between μQFR and 3D-QFR, resulting in no single false positive or negative. Kappa index was 1 and the diagnostic accuracy 100%.
Conclusions
μQFR using a single angiographic projection showed almost perfect agreement with standard 3D-QFR. These results encourage the interchangeable use of μQFR and 3D-QFR, which can be interesting to improve QFR feasibility in retrospective studies, wherein appropriate double angiographic projections might be challenging to obtain.
Related collections
Most cited references26
- Record: found
- Abstract: not found
- Article: not found
2018 ESC/EACTS Guidelines on myocardial revascularization
- Record: found
- Abstract: found
- Article: not found
Fractional flow reserve versus angiography for guiding percutaneous coronary intervention.
- Record: found
- Abstract: found
- Article: not found