- Record: found
- Abstract: found
- Article: found
Adipose derived mesenchymal stem cells transplantation via portal vein improves microcirculation and ameliorates liver fibrosis induced by CCl4 in rats
Read this article at
Abstract
Introduction
Adipose derived mesenchymal stem cells (ADMSCs), carrying the similar characteristics to bone marrow mesenchymal stem cells, only much more abundant and easier to obtain, may be a promising treatment for liver fibrosis. We aim to investigate the therapeutic potential of ADMSCs transplantation in liver fibrosis caused by carbon tetrachloride (CCl 4) in rats as well as its underlying mechanism, and to further explore the appropriate infusion pathway.
Methods
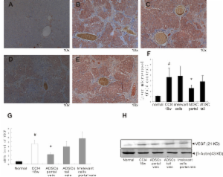
ADMSCs were isolated, cultured and identified. Placebo and ADMSCs were transplanted via portal vein and tail vein respectively into carbon tetrachloride (CCl 4)-induced liver fibrosis rats. Computed tomography (CT) perfusion scan and microvessel counts were performed to measure the alteration of liver microcirculation after therapy. Liver function tests and histological findings were estimated.
Results
CT perfusion scan shown significant decrease of hepatic arterial perfusion index, significant increased portal vein perfusion, total liver perfusion in rats receiving ADMSCs from portal vein, and Factor VIII (FVIII) immunohistochemical staining shown significant decrease of microvessels in rats receiving ADMSCs from portal vein, indicating microcirculation improvement in portal vein group. Vascular endothelial growth Factor (VEGF) was significantly up-regulated in fibrosis models, and decreased after ADMSCs intraportal transplantation. A significant improvement of liver functional test and histological findings in portal vein group were observed. No significance was found in rats receiving ADMSCs from tail vein.
Conclusions
ADMSCs have a therapeutic effect against CCl 4-mediated liver fibrosis. ADMSCs may benefit the fibrotic liver through alteration of microcirculation, evidenced by CT perfusion scan and down-regulation of VEGF. Intraportal transplantation is a better pathway than tail vein transplantation.
Related collections
Most cited references42
- Record: found
- Abstract: found
- Article: not found
In vitro hepatic differentiation of human mesenchymal stem cells.
- Record: found
- Abstract: found
- Article: not found
Mesenchymal stem cells: biology and potential clinical uses.
- Record: found
- Abstract: found
- Article: not found