- Record: found
- Abstract: found
- Article: found
Comparative study analyzing survival and safety of bevacizumab/carboplatin/paclitaxel and cisplatin/pemetrexed in chemotherapy-naïve patients with advanced non-squamous bronchogenic carcinoma not harboring EGFR mutation
Abstract
Purpose
The majority of Egyptian patients with lung cancer present at a late stage of the disease. Bevacizumab/carboplatin/paclitaxel, as well as cisplatin plus pemetrexed, are both standard regimens for advanced non-squamous bronchogenic cancer. This study compares both regimens, in terms of efficacy and toxicity profile, in Egyptian patients.
Patients and methods
This is a randomized Phase II study comparing toxicity profile and survival in 41 chemotherapy-naïve patients with stage IIIB or IV non-squamous NSCLC, with an ECOG performance status of 0 to 2. The epidermal growth factor receptor (EGFR) mutation detection was performed prior to treatment of all patients. Patients in the first group received: bevacizumab 7.5 mg/m 2 on Day 1 and Day 15; carboplatin area under the curve-5 on Day 1; and paclitaxel 60 mg/m 2 on Day 1, Day 8, and Day 15 every 4 weeks. In the second group, patients received cisplatin 75 mg/m 2 and pemetrexed 500 mg/m 2 every 3 weeks.
Results
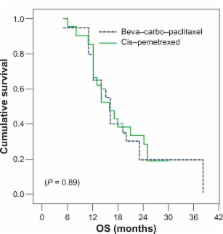
The combination of bevacizumab/carboplatin/paclitaxel demonstrated higher Grade III–IV toxicity than cisplatin/pemetrexed regarding sensory/motor neuropathy ( P = 0.06), DVT ( P = 0.23), proteinuria ( P = 0.23), and hypertension ( P = 0.11), as well as Grade II alopecia ( P = 0.001); however, no significant difference in toxicities between both arms was recorded regarding nausea and vomiting ( P = 0.66), hematological toxicity, febrile neutropenia ( P = 1) and fatigue ( P = 0.66). Progression-free survival was similar for both treatment arms with a median of 6 months ( P = 0.978). Overall median survival was comparable in both arms, 16.07 months versus 16.01 months ( P = 0.89).
Conclusion
Bevacizumab/carboplatin/paclitaxel and cisplatin/pemetrexed provided meaningful and comparable efficacy in advanced non-squamous bronchogenic carcinoma not harboring EGFR mutation. No significant difference in toxicity was observed between both treatment arms, apart from bevacizumab/carboplatin/paclitaxel-related risks as DVT, hypertension, proteinuria, sensory/motor neuropathy, and alopecia.
Most cited references17
- Record: found
- Abstract: found
- Article: not found
Prediction of creatinine clearance from serum creatinine.
- Record: found
- Abstract: found
- Article: not found
Phase III study of pemetrexed in combination with cisplatin versus cisplatin alone in patients with malignant pleural mesothelioma.
- Record: found
- Abstract: found
- Article: not found