- Record: found
- Abstract: found
- Article: found
Acute Gonococcal Conjunctivitis in Adolescent Teenager: A Case Report
letter
Read this article at
There is no author summary for this article yet. Authors can add summaries to their articles on ScienceOpen to make them more accessible to a non-specialist audience.
Abstract
Dear Editor,
Gonococcal conjunctivitis is typically a neonatal disease. However, the incidence
of gonococcal conjunctivitis in adults is increasing because of the increased frequency
of urogenital gonococcal infections [1]. Most cases occur in neonates or sexually
active adults. It is rarely considered in older children or adolescents. Since it
is relatively rare in adolescents, clinical diagnosis may be delayed [2,3]. Inappropriate
treatment timing means that gonococcal conjunctivitis could progress in a rapid and
fulminant fashion, threatening patients’ vision. If systemic antibiotic therapy and
topical eye-drop treatment are instituted before severe corneal complications occur,
serious sequelae and visual loss could be reduced. We report a rare case of acute
gonococcal conjunctivitis in an adolescent teenager diagnosed using a bacterial culture
test without any ocular complications. The patient provided informed consent for the
publication of clinical photographs.
A 13-year-old adolescent boy presented with severe eyelid swelling and ocular pain
with purulent discharge from the left eye, which started 5 days before presentation.
The best-corrected visual acuity (BCVA) of the right eye was 20/20 and that of the
left eye was 20/400. Severely decreased visual acuity of the left eye was observed.
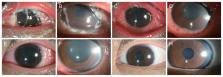
Slitlamp examination revealed unremarkable findings in the right eye; however, the
left eye showed severe chemosis with conjunctival injection, vessel dilatation, and
multiple tarsal conjunctival follicles. Diffuse superficial punctate corneal lesions
with hazy and mild edema and purulent discharge in the conjunctival sac were also
observed (Fig. 1A, 1B). The patient denied a history of sexual contact and showed
no evidence of genitourinary symptoms. However, because gonococcal conjunctivitis
was strongly suspected, bacterial culture using a disinfectant swab was performed
at the first visit, and other laboratory examinations and urine analyses were performed.
This patient, with gram-negative intracellular diplococci on Gram stain, subsequently
had positive conjunctival cultures for Neisseria gonorrhoeae. Other blood markers
of inflammation, such as C-reactive protein and erythrocyte sedimentation rate, were
slightly elevated, but urinalysis results were normal.
The patient was administered a single dose of 1 g of intravenous ceftazidime (Cefazim,
HK inno.N) and 500 mg azithromycin (Zithromax, Pfizer Inc) orally twice a day for
5 days. Topical fortified tobramycin and cephalosporin eye drops were instilled every
1 hour. Within a day, the patient showed reduced ocular discharge and inflamed conjunctiva
(Fig. 1C, 1D). Topical fortified eyedrops were tapered and used every 2 hours. After
5 days, the BCVA of the left eye was 20/50, and conjunctival injection and corneal
haziness improved (Fig. 1E, 1F). The patient was discharged after 5 days of treatment.
Topical fortified eyedrops were used four times a day. After 2 weeks, the left eye
BCVA was 20/20, and eyelid swelling, corneal haziness, and conjunctival injection
were mostly reduced; corneal edema remained slight. Topical fortified eyedrops were
stopped, and the patient was switched to levofloxacin eye drops. Three weeks after
discharge, the patient had a visual acuity of 20/20 in the left eye without any conjunctival
or corneal complications (Fig. 1G, 1H).
To our knowledge, this is the first report of acute gonococcal conjunctivitis in an
adolescent in Korea. The patient reported no history of sexual contact. Nevertheless,
the clinical symptoms strongly suggested the possibility of N. gonorrhoeae conjunctivitis.
There have been reports of nonsexual transmission of gonococcal infection in an 11-year-old
girl by a thermal pool [4]. In adolescent patients, sexual abuse should always be
the first consideration and should be investigated. No evidence of sexual assault
or other sexually transmitted infections was found in the urinalysis or genitourinary
evaluations. Many studies have been conducted to determine the survival time of gonococci
on several materials, such as towels and sheets. Gonococcus was found in almost all
materials after 24 to 48 hours and survive up to 72 hours or more on certain materials
[5]. In previous report, gonococcal conjunctivitis did not necessarily require sexual
contact as an antecedent factor [4,5]. Therefore, if gonococcal conjunctivitis is
strongly suspected, a conjunctival culture test to confirm gonococci can be helpful
in the diagnosis.
In conclusion, acute gonococcal conjunctivitis can be observed in young adolescents
who are sexually inactive. Therefore, conjunctival swap culture helps diagnose gonococcal
infection and conjunctivitis presenting with severe purulent discharge. Systemic intravenous
third-generation cephalosporin and oral azithromycin intake were effective in relieving
the symptoms of gonococcal conjunctivitis.
Related collections
Most cited references5
- Record: found
- Abstract: not found
- Article: not found
Diagnosis and Treatment of Sexually Transmitted Infections: A Review
Susan Tuddenham, Matthew M Hamill, Khalil Ghanem (2022)
- Record: found
- Abstract: not found
- Article: not found
What is the evidence for non-sexual transmission of gonorrhoea in children after the neonatal period? A systematic review
Felicity Goodyear-Smith (2007)

- Record: found
- Abstract: found
- Article: found