- Record: found
- Abstract: found
- Article: found
Case 4/2017 - Double-Chambered Right Ventricle with Dextrocardia and Hypoxemia Due to Atrial Shunt in a 4-Year-Old Girl
case-report
Read this article at
There is no author summary for this article yet. Authors can add summaries to their articles on ScienceOpen to make them more accessible to a non-specialist audience.
Abstract
Clinical data
A premature female twin (33-week gestation), weighing at birth 1935 g, remained
hospitalized for one month due to the diagnosis of atrial septal defect (ASD) +
ventricular septal defect (VSD) + persistence of ductus arteriosus (PDA). The
patient gained less weight than the average children, but maintained full and
similar activity, receiving furosemide and captopril, up to the age of 3 years, when
her mother noticed cyanosis.
Physical exam
Eupnea; mild cyanosis; normal pulses; weight, 11 kg; height, 89 cm; heart rate,
100 bpm; O2 saturation, 83%. The aorta was not palpable at the
suprasternal notch. Her chest showed mild bulging and mild systolic thrusts on
the right sternal border (RSB). The 1st heart sound was more intense
on the right midclavicular line (RMCL), and the 2nd heart sound, on
the RSB with greater radiation to the RMCL. A rough systolic ejection murmur
(4/6) was audible on the upper RSB, and a mild regurgitation systolic murmur
(4/6) was audible on the lower RSB. The liver was palpated 1 cm from the right
costal margin.
Complementary diagnostic tests
Electrocardiogram: sinus rhythm and signs of marked right
ventricular overload. There were Rs complexes in V1 to V3, rsR´ in V5R and V6R,
positive T wave in V1 to V6, and isoelectric T wave in V6R, signs of right
ventricle (RV) located to the right. AP: +60º, AQRS: -150º, AT: +70º (Figure1).
Figure 1
X-ray showing marked cardiomegaly with rounded and long ventricular
arch to the right, situs solitus (gastric bubble to the left) and
reduced pulmonary vascular bed. Electrocardiogram showing signs of
marked right ventricular overload to the right, with preponderant R
wave in V6R, S wave in V6, positive T wave in V6, and isoelectric T
wave in V6R.
Chest X-ray: enlargement of the cardiac silhouette to the right, and
reduced pulmonary vascular bed. Rounded and long ventricular arch to the right
(Figure1).
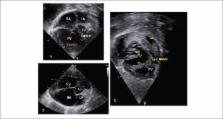
Echocardiogram: (Figure2)
showed situs solitus with dextrocardia, normal systemic and pulmonary venous
connections, concordant atrioventricular and ventriculoarterial connections.
Dilatation of the inferior vena cava and suprahepatic veins. Ostium secundum ASD
of 4 mm, with right-to-left shunt. Intact ventricular septum deviated to the
left. Marked tricuspid regurgitation. Aneurysmatic right atrium with volume of
58 mL/m2. Right ventricle markedly dilated and hypertrophied, with
hypertrophied moderator band, narrow infundibulum due to hypertrophy, and two
ventricular chambers with a 140-mmHg gradient between them. Normal pulmonary and
aortic valves. Normal left cavities. PT = 20 mm, PA´s = 9 mm. Pulmonary ring =
15 mm and right ventricular anterior wall = 10 mm.
Figure 2
Echocardiogram: 4-chamber (A) and short-axis (B) views showing
markedly enlarged right cardiac cavities with septa bulging to the
left and marked ventricular hypertrophy (arrows), and moderator band
dividing the two right ventricular chambers: proximal and distal
chambers seen on subcostal view (C). RA: right atrium; LA: left
atrium; Ao: aorta; RV: right ventricle; LV: left ventricle; PA:
pulmonary artery.
Clinical diagnosis
Stenosis of double-chambered right ventricular inlet with mild hypoxia due to
right-to-left shunt through a small ASD.
Clinical rationale
The clinical elements were compatible with cyanotic congenital heart disease with
reduced pulmonary flow resulting from an obstruction at the right and
right-to-left shunt. An obstruction in the right ventricular inlet could be
suspected based on the auscultation of a markedly rough and intense systolic
murmur. However, the more intense 2nd heart sound raised the
possibility of corrected transposition of the great arteries, mainly in the
presence of dextrocardia with situs solitus. The electrocardiogram was not
compatible with atrioventricular discordance, because the T wave indicated a RV
located to the right (T wave axis to the left (+70 degrees) and greater
intensity in V6 than in V6R). The echocardiogram was conclusive about the defect
and its repercussion. The marked tricuspid regurgitation causing an aneurysmatic
right atrium was due to marked obstruction inside the RV. It is worth noting the
rarity of that anomaly in the presence of dextrocardia with situs solitus and no
VSD, in addition to marked tricuspid regurgitation as an uncommon consequence
from obstruction in the RV.
Differential diagnosis
The most likely differential diagnosis was corrected transposition of the great
arteries.
Management
Because of the marked repercussion of the defect, surgery was performed
immediately, eliminating the obstruction of the inlet of the hypertrophied
RV.
Comments
The double-chambered RV or stenosis of the inlet of the RV is a rare congenital
anomaly, in which an anomalous hypertrophied muscular band divides the RV into two
cavities, the proximal being of high pressure, and the distal, of low pressure.
Muscular obstruction develops over time, but rarely in adult age. The hypertrophied
muscle is either the septoparietal or the septomarginal trabecula.
In over 95% of the cases, the stenosis of the inlet of the RV is associated with VSD,
whose location determines the characteristic clinical findings. Thus, when the VSD
is located before the obstruction, the clinical findings are similar to those of
tetralogy of Fallot, and when the VSD is distal to the obstruction, those findings
are similar to those of the VSD itself. It is worth noting that the grade of
obstruction and the size of the VSD account for the magnitude of the findings.
To our knowledge, this is the first report on the association of double-chambered
RV
with dextrocardia and situs solitus and no VSD, whose clinical findings simulated
those of marked pulmonary stenosis and consequent progressive tricuspid
regurgitation.
1,2
Related collections
Most cited references2
- Record: found
- Abstract: found
- Article: not found
Long-term natural history and postoperative outcome of double-chambered right ventricle—Experience from two tertiary adult congenital heart centres and review of the literature
- Record: found
- Abstract: found
- Article: not found
Surgical Outcomes and Postoperative Prognosis Beyond 10 Years for Double-Chambered Right Ventricle
Masashi Amano, Chisato Izumi, Yukiko Hayama … (2015)