- Record: found
- Abstract: found
- Article: found
Cognitive clustering in schizophrenia patients, their first-degree relatives and healthy subjects is associated with anterior cingulate cortex volume
Read this article at
Abstract
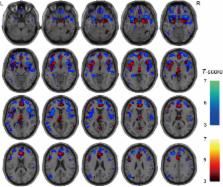
Cognitive impairments are a core feature in schizophrenia patients (SCZ) and are also observed in first-degree relatives (FR) of SCZ. However, substantial variability in the impairments exists within and among SCZ, FR and healthy controls (HC). A cluster-analytic approach can group individuals based on profiles of traits and create more homogeneous groupings than predefined categories. Here, we investigated differences in the Brief Assessment of Cognition in Schizophrenia (BACS) neuropsychological battery (six subscales) among SCZ, unaffected FR and HC. To identify three homogeneous and meaningful cognitive groups regardless of categorical diagnoses (SCZ, FR and HC), cognitive clustering was performed, and differences in the BACS subscales among the cognitive cluster groups were investigated. Finally, the effects of diagnosis and cognition on brain volumes were examined. As expected, there were significant differences in the five BACS subscales among the diagnostic groups. The cluster-analytic approach generated three meaningful subgroups: (i) neuropsychologically normal, (ii) intermediate impaired and (iii) widespread impaired. The cognitive subgroups were mainly affected by the clinical diagnosis, and significant differences in all BACS subscales among clusters were found. The effects of the diagnosis and cognitive clusters on brain volumes overlapped in the frontal, temporal and limbic regions. Frontal and temporal volumes were mainly affected by the diagnosis, whereas the anterior cingulate cortex (ACC) volumes were affected by the additive effects of diagnosis and cognition. Our findings demonstrate a cognitive continuum among SCZ, FR and HC and support the concept of cognitive impairment and the related ACC volumes as intermediate phenotypes in SCZ.
Highlights
-
•
Cognitive impairments in the BACS subscales were a continuum among SCZ, FR and HC.
-
•
Cognitive clustering based on the BACS regardless of clinical diagnosis was performed.
-
•
Neuropsychologically normal, intermediately impaired and widespread impaired cognitive clusters were identified.
-
•
The cognitive clusters were mainly affected by the clinical diagnosis (SCZ, FR and HC).
-
•
Frontal and temporal volumes were mainly affected by the diagnosis.
-
•
The ACC volumes were affected by the additive effects of diagnosis and cognition.
Related collections
Most cited references46
- Record: found
- Abstract: found
- Article: not found
The positive and negative syndrome scale (PANSS) for schizophrenia.
- Record: found
- Abstract: found
- Article: not found
What are the functional consequences of neurocognitive deficits in schizophrenia?
- Record: found
- Abstract: found
- Article: not found