- Record: found
- Abstract: found
- Article: found
Association between Elevated Pleural Interleukin-33 Levels and Tuberculous Pleurisy
Read this article at
Abstract
Background
Interferon-γ (IFN-γ) plays a crucial role in Mycobacterium tuberculosis induced pleural responses. Interleukin (IL)-33 up-regulates the production of IFN-γ. We aimed to identify whether an association between pleural IL-33 levels and tuberculous pleurisy exists and determine its diagnostic value.
Methods
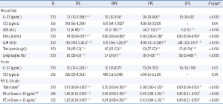
Pleural IL-33, ST2 (a receptor of IL-33), adenosine deaminase (ADA), and IFN-γ, as well as serum IL-33 and ST2 were measured in 220 patients with pleural effusions (PEs). Patients with malignant (MPEs), parapneumonic (PPEs), tuberculous (TPEs), and cardiogenic (CPEs) pleural effusions were included.
Results
Pleural and serum IL-33 levels were highest or tended to be higher in patients with TPEs than in those with other types of PEs. The median pleural fluid-to-serum IL-33 ratio was higher in TPE cases (≥ 0.91) than in other PE cases (≤ 0.56). Pleural IL-33 levels correlated with those of pleural ADA and IFN-γ. However, the diagnostic accuracies of pleural IL-33 (0.74) and pleural fluid-to-serum IL-33 ratio (0.75) were lower than that of ADA (0.95) or IFN-γ (0.97). Pleural ST2 levels in patients with MPEs were higher than in patients with TPEs. Serum ST2 levels did not differ among the groups.
Related collections
Most cited references30

- Record: found
- Abstract: found
- Article: found
Role of IL-33 in inflammation and disease
- Record: found
- Abstract: found
- Article: not found