- Record: found
- Abstract: found
- Article: found
Ruxolitinib-treated polycythemia vera patients and their risk of secondary malignancies

Read this article at
Abstract
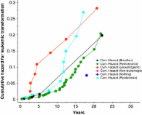
Recently, there has been increased concern about a risk of secondary malignancies (SM) occurring in myelofibrosis (MF) patients receiving ruxolitinib (RUX). In polycythemia vera (PV), on the other hand, only limited data on the risk of SM under RUX treatment are available. To investigate the association between RUX therapy in PV and SM, we conducted a retrospective, single-center study that included 289 PV patients. RUX was administered to 32.9% (95/289) of patients for a median treatment duration of 48.0 months (range 1.0–101.6). Within a median follow-up of 97 months (1.0–395.0) after PV diagnosis, 24 SM occurred. Comparing the number of PV patients with RUX-associated SM ( n = 10, 41.7%) with the 14 (58.3%) patients who developed SM without RUX, no significant difference ( p = 0.34, chi square test) was found. No increased incidences of melanoma, lymphoma, or solid “non-skin” malignancies were observed with RUX ( p = 0.31, p = 0.60, and p = 0.63, respectively, chi square test). However, significantly more NMSC occurred in association with RUX treatment ( p = 0.03, chi-squared test). The “SM-free survival” was not significantly different by log rank test for all 289 patients ( p = 0.65), for the patients ( n = 208; 72%) receiving cytoreductive therapy ( p = 0.48) or for different therapy sequences ( p = 0.074). In multivariate analysis, advanced age at PV diagnosis (HR 1.062 [95% CI 1.028, 1.098]) but not administration of RUX (HR 1.068 [95% CI 0.468, 2.463]) was associated with an increased risk for SM ( p = 0.005). According to this retrospective analysis, no increased risk of SM due to RUX treatment could be substantiated for PV.
Related collections
Most cited references22
- Record: found
- Abstract: found
- Article: not found
The 2008 revision of the World Health Organization (WHO) classification of myeloid neoplasms and acute leukemia: rationale and important changes.

- Record: found
- Abstract: found
- Article: found
The 2016 WHO classification and diagnostic criteria for myeloproliferative neoplasms: document summary and in-depth discussion
- Record: found
- Abstract: found
- Article: found