- Record: found
- Abstract: found
- Article: found
Healthcare Resource Utilization and Direct Cost of Patients with Atopic Dermatitis in Dubai, United Arab Emirates: A Retrospective Cohort Study
Read this article at
Abstract
Introduction
Atopic dermatitis (AD) data are scarce in Dubai [United Arab Emirates (UAE)]. Therefore, this study aimed at understanding real-world healthcare resource utilization (HCRU) and related costs, specialties, treatment landscape, consultation-based prevalence and incidence, and patient characteristics.
Methods
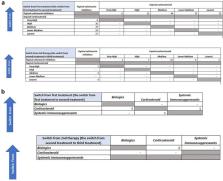
This retrospective, longitudinal, insurance e-claims (Dubai Private Insurance—insured expatriates) database studied AD in Dubai between 1 January 2014 and 31 March 2020. Two cohorts of patients based on treatment status as the eligibility criteria were selected from 442,956 patients with at least two AD diagnosis claims: treated AD [mild to moderate (10,134 patients) and moderate to severe (3515 patients)] and untreated or on drugs not included in the treated AD cohort (10,806 patients).
Results
Across treated AD (mild to moderate and moderate to severe) and untreated AD cohorts, mean age was ~ 29 years; the majority were from dermatology (65–44%) and pediatrics (29–32%) specialty. Key HCRU cost contributors were hospitalizations and outpatient visits in both the treated AD groups. Mean annual disease-specific HCRU cost per patient was highest for the moderate-to-severe treated (531.5 USD) cohort, followed by the mild-to-moderate treated (378.4 USD) cohort, and lowest for the untreated (144.0 USD) cohort; patients with AD with any infection, asthma, or allergic rhinitis showed a similar trend. However, AD-diagnosed patients with Staphylococcus infection had the highest mean HCRU cost among the mild-to-moderate treated AD cohort, followed by the moderate-to-severe treated AD cohort.
Conclusion
This study indicated AD to be a common skin disease with a prevalence rate of 4–5% in Dubai (UAE), with the majority of patients (about 90%) being treated by specialists. However, there is a significant underuse of newer innovative therapies (including biologics). Also, disease severity (moderate-to-severe AD) was associated with high direct medical cost, which could be controlled by early intervention. Furthermore, AD treatment choice could focus on major direct HCRU cost contributors such as hospitalizations, comorbid conditions, and infections.
Related collections
Most cited references55
- Record: found
- Abstract: found
- Article: not found
Atopic dermatitis
- Record: found
- Abstract: found
- Article: found
Atopic Dermatitis: Global Epidemiology and Risk Factors

- Record: found
- Abstract: found
- Article: found