- Record: found
- Abstract: found
- Article: not found
Veno-venous extra-corporeal membrane oxygenation in a COVID-19 patient with cold-agglutinin haemolytic anaemia: A case report
Read this article at
Abstract
Overview
The use of extra-corporeal membrane oxygenation (ECMO) therapy to treat severe COVID-19 patients with acute respiratory failure is increasing worldwide. We reported herein the use of veno-venous ECMO in a patient with cold agglutinin haemolytic anaemia (CAHA) who suffered from severe COVID-19 infection.
Description
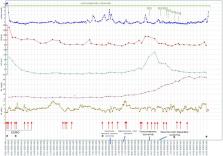
A 64-year-old man presented to the emergency department (ED) with incremental complaints of dyspnoea and cough since one week. His history consisted of CAHA, which responded well to corticosteroid treatment. Because of severe hypoxemia, urgent intubation and mechanical ventilation were necessary. Despite deep sedation, muscle paralysis and prone ventilation, P/F ratio remained low. Though his history of CAHA, he still was considered for VV-ECMO. As lab results pointed to recurrence of CAHA, corticosteroids and rituximab were started. The VV-ECMO run was short and rather uncomplicated. Although, despite treatment, CAHA persisted and caused important complications of intestinal ischemia, which needed multiple surgical interventions. Finally, the patient suffered from progressive liver failure, thought to be secondary to ischemic cholangitis. One month after admission, therapy was stopped and patient passed away.
Related collections
Most cited references12

- Record: found
- Abstract: found
- Article: found
Extracorporeal membrane oxygenation for COVID-19: a systematic review and meta-analysis
- Record: found
- Abstract: found
- Article: not found
Cold agglutinin disease.
- Record: found
- Abstract: not found
- Article: not found
