- Record: found
- Abstract: found
- Article: found
Baseline Splenic Volume as a Prognostic Biomarker of FOLFIRI Efficacy and a Surrogate Marker of MDSC Accumulation in Metastatic Colorectal Carcinoma
Read this article at
Abstract
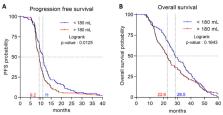
Background: Predictive biomarkers of response to chemotherapy plus antiangiogenic for metastatic colorectal cancer (mCRC) are lacking. The objective of this study was to test the prognostic role of splenomegaly on baseline CT scan. Methods: This study is a sub-study of PRODIGE-9 study, which included 488 mCRC patients treated by 5-fluorouracil, leucovorin and irinotecan (FOLFIRI) and bevacizumab in first line. The association between splenic volume, and PFS and OS was evaluated by univariate and multivariable Cox analyses. The relation between circulating monocytic Myeloid derived suppressor cells (mMDSC) and splenomegaly was also determined. Results: Baseline splenic volume > 180 mL was associated with poor PFS (median PFS = 9.2 versus 11.1 months; log-rank p = 0.0125), but was not statistically associated with OS (median OS = 22.6 versus 28.5 months; log-rank p = 0.1643). The increase in splenic volume at 3 months had no impact on PFS (HR 0.928; log-rank p = 0.56) or on OS (HR 0.843; log-rank p = 0.21). Baseline splenic volume was positively correlated with the level of baseline circulating mMDSC ( r = 0.48, p-value = 0.031). Conclusion: Baseline splenomegaly is a prognostic biomarker in patients with mCRC treated with FOLFIRI and bevacizumab, and a surrogate marker of MDSC accumulation.
Related collections
Most cited references29
- Record: found
- Abstract: not found
- Article: not found
Metastatic colorectal cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up.
- Record: found
- Abstract: found
- Article: not found
Initial therapy with FOLFOXIRI and bevacizumab for metastatic colorectal cancer.
- Record: found
- Abstract: found
- Article: not found