- Record: found
- Abstract: found
- Article: found
GnRH agonist versus GnRH antagonist in assisted reproduction cycles: oocyte morphology

Read this article at
Abstract
Background
The selection of developmentally competent human gametes may increase the efficiency of assisted reproduction. Spermatozoa and oocytes are usually assessed according to morphological criteria. Oocyte morphology can be affected by the age, genetic characteristics, and factors related to controlled ovarian stimulation. However, there is a lack of evidence in the literature concerning the effect of gonadotropin-releasing hormone (GnRH) analogues, either agonists or antagonists, on oocyte morphology. The aim of this randomized study was to investigate whether the prevalence of oocyte dysmorphism is influenced by the type of pituitary suppression used in ovarian stimulation.
Methods
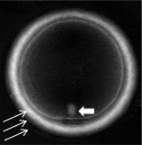
A total of 64 patients in the first intracytoplasmic sperm injection (ICSI) cycle were prospectively randomized to receive treatment with either a GnRH agonist with a long-term protocol (n: 32) or a GnRH antagonist with a multi-dose protocol (n: 32). Before being subjected to ICSI, the oocytes at metaphase II from both groups were morphologically analyzed under an inverted light microscope at 400x magnification. The oocytes were classified as follows: normal or with cytoplasmic dysmorphism, extracytoplasmic dysmorphism, or both. The number of dysmorphic oocytes per total number of oocytes was analyzed.
Results
Out of a total of 681 oocytes, 189 (27.8 %) were morphologically normal, 220 (32.3 %) showed cytoplasmic dysmorphism, 124 (18.2%) showed extracytoplasmic alterations, and 148 (21.7%) exhibited both types of dysmorphism. No significant difference in oocyte dysmorphism was observed between the agonist- and antagonist-treated groups ( P ≫ 0.05). Analysis for each dysmorphism revealed that the most common conditions were alterations in polar body shape (31.3%) and the presence of diffuse cytoplasmic granulations (22.8%), refractile bodies (18.5%) and central cytoplasmic granulations (13.6%). There was no significant difference among individual oocyte dysmorphisms in the agonist- and antagonist-treated groups ( P ≫ 0.05).
Conclusions
Our randomized data indicate that in terms of the quality of oocyte morphology, there is no difference between the antagonist multi-dose protocol and the long-term agonist protocol. If a GnRH analogue used for pituitary suppression in IVF cycles influences the prevalence of oocyte dysmorphisms, there does not appear to be a difference between the use of an agonist as opposed to an antagonist.
Related collections
Most cited references62
- Record: found
- Abstract: found
- Article: found
Predictive value of oocyte morphology in human IVF: a systematic review of the literature
- Record: found
- Abstract: found
- Article: not found