- Record: found
- Abstract: found
- Article: found
Development of a Fast Onset Proton Pump Inhibitor: Comparison of Fixed-Dose Combination of Rabeprazole and Sodium Bicarbonate (YPI-011) to the Conventional Enteric-Coated Rabeprazole
Abstract
Purpose
Proton pump inhibitors (PPIs) are the first-line therapy for gastroesophageal reflux disorder (GERD). Unlike conventional PPIs, non-enteric coated PPIs with antacid salt enable a faster acid suppression through the rapid absorption of the PPI. YPI-011 is a newly developed fixed-dose combination of a rabeprazole with sodium bicarbonate (NaHCO 3). This study compared the pharmacokinetics (PKs) and pharmacodynamics (PDs) of YPI-011 to the conventional enteric-coated rabeprazole (Pariet ®).
Materials and Methods
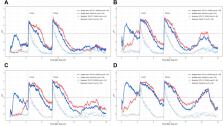
A randomized, open-label, two-treatment, two-sequence crossover study was conducted with two different doses (10 and 20 mg) and 44 subjects in each group. They randomly received either a test or reference treatment for 7 days in the first period and the other treatment in the second period. Blood samples for the PK analysis were taken after the single- and multiple-dose. Intragastric pH monitoring for the PD analysis was implemented for baseline and after the single- and multiple-dose.
Results
Gastric acid suppression evaluated by the percentage decrease from baseline in the integrated gastric acidity for a 24-hour interval after the multiple-dose was similar between the treatments in both dose groups. The systemic exposure of rabeprazole at steady state after the multiple-dose was also similar between the treatments in both dose groups. The time to reach the maximum rabeprazole concentration was faster in the test treatment. The PK-PD relationship of PPI is well known, and the faster absorption of rabeprazole resulted in a more rapid mode of action in acid suppression.
Most cited references21
- Record: found
- Abstract: found
- Article: not found
The Montreal definition and classification of gastroesophageal reflux disease: a global evidence-based consensus.
- Record: found
- Abstract: found
- Article: not found
Clinical Pharmacogenetics Implementation Consortium (CPIC) Guideline for CYP2C19 and Proton Pump Inhibitor Dosing.
- Record: found
- Abstract: found
- Article: not found