- Record: found
- Abstract: found
- Article: found
A double-blind randomised placebo-controlled trial investigating the effects of lesogaberan on the objective cough frequency and capsaicin-evoked coughs in patients with refractory chronic cough
Read this article at
Abstract
Objective
Baclofen is a centrally acting γ-aminobutyric acid type B (GABA B) receptor agonist which reduces gastro-oesophageal reflux and suppresses the cough reflex; however, central nervous system side-effects limit its use. Lesogaberan is a novel peripherally acting GABA B agonist, but its effects on refractory chronic cough are unknown.
Design
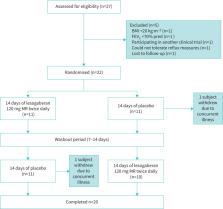
We performed a single-centre, placebo-controlled, double-blind randomised crossover study in patients with chronic cough, refractory to the treatment of underlying conditions. Patients were randomised to treatment with lesogaberan 120 mg modified release twice daily or matched placebo for 2 weeks and then crossed over to the alternative therapy after a 2-week washout. The primary end-point was 24-h cough frequency measured with an acoustic monitoring system. In addition, cough responses to capsaicin were measured, and gastro-oesophageal reflux assessed by 24-h pH/impedance at screening.
Results
22 patients were randomised to receive lesogaberan/placebo or placebo/lesogaberan (female (73%); mean± sd age 63.7±7.2 years; median (interquartile range) cough duration 10.5 (5.8–17.0) years; mean (95% CI) 45 (29–67) reflux events in 24 h; two patients had abnormal oesophageal acid exposure times). Although lesogaberan reduced cough counts by 26% over placebo, this did not reach statistical significance (p=0.12). However, lesogaberan did significantly improve cough responses to capsaicin (p=0.04) and the number of cough bouts (p=0.04) compared with placebo. Lesogaberan was well tolerated in this study.
Abstract
Lesogaberan, a peripherally acting GABA B agonist, does not reduce 24-h cough frequency in patients with chronic cough despite significantly reducing capsaicin-induced coughing https://bit.ly/3uGyPQL
Related collections
Most cited references39
- Record: found
- Abstract: found
- Article: not found
The Chicago Classification of esophageal motility disorders, v3.0.
- Record: found
- Abstract: found
- Article: not found
ERS guidelines on the diagnosis and treatment of chronic cough in adults and children
- Record: found
- Abstract: not found
- Article: not found