- Record: found
- Abstract: found
- Article: found
TFE3-associated perivascular epithelioid cell tumor with complete response to mTOR inhibitor therapy: report of first case and literature review
Read this article at
Abstract
Background
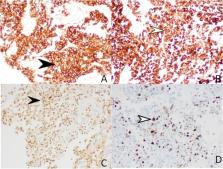
Perivascular epitheloid cell tumor (PEComas) are characterized by expression of both muscles, most often smooth muscle actin (in ~80% of cases) and melanocytic markers (mainly HMB-45 and Melan A). TFE 3-associated PEComas are new variant which are poorly defined due to their limited reports in literature. These tumors lack response to targeted mTOR inhibitor therapy due to lack of mutation in TSC gene. Hereby, we are reporting a case of TFE3 associated pelvic PEComa showing excellent response to Everolimus.
Case presentation
A 45-year-old female presented with complaint of abdominal mass and bleeding per vaginum for 4 months. She had a history of total abdominal hysterectomy 3 years back in view of abnormal uterine bleeding and exploratory laprotomy 7 months back to remove some pelvic mass. Imaging suggested of ill-defined heterogenous mass of 9.3 x 9.2 x 16 cm involving the uterus, cervix, and upper 1/3 vagina. Multiple omental and peritoneal deposits were also seen, making probable diagnosis of carcinoma endometrium. USG guided biopsy showed cores of fibrous tissue with the presence of cells in sheets with granular eosinophillic cytoplasm; IHC showed positivity for TFE-3, H Caldesmon, GATA-3, and Melan A- and HMB-45; and Ki 67 index was 35%. The basis of above diagnosis of PEComa was made and she was started on Everolimus; repeat imaging after 3 months of therapy showed complete response.
Related collections
Most cited references19
- Record: found
- Abstract: found
- Article: not found
Integrative genomic analyses identify MITF as a lineage survival oncogene amplified in malignant melanoma.
- Record: found
- Abstract: found
- Article: not found
Perivascular epithelioid cell neoplasms of soft tissue and gynecologic origin: a clinicopathologic study of 26 cases and review of the literature.
- Record: found
- Abstract: found
- Article: not found
Uterine PEComas: A Morphologic, Immunohistochemical, and Molecular Analysis of 32 Tumors
Author and article information
Comments
Comment on this article
 Smart Citations
Smart CitationsSee how this article has been cited at scite.ai
scite shows how a scientific paper has been cited by providing the context of the citation, a classification describing whether it supports, mentions, or contrasts the cited claim, and a label indicating in which section the citation was made.