- Record: found
- Abstract: found
- Article: not found
Intrascleral outflow after deep sclerectomy with absorbable and non-absorbable implants in the rabbit eye
Read this article at
Summary
Background
The purpose of the study is an analysis of intrascleral drainage vessels formed in rabbits’ eyes after non-penetrating deep sclerectomy (NPDS) with absorbable and non-absorbable implants, and comparison to eyes in which surgery was performed without implanted material.
Material/Methods
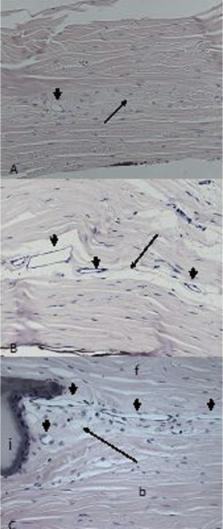
NPDS was carried out in 12 rabbits, with implantation of non-absorbable methacrylic hydrogel (N=10 eyes) or absorbable cross-linked sodium hyaluronate (N=6 eyes), or without any implant (N=8 eyes). All the animals were euthanized 1 year after surgery. Twenty-one eyeballs were prepared for light microscopy and 3 were prepared for transmission electron microscope (TEM) analysis. Aqueous humour pathways were stained with ferritin in 6 eyeballs.
Results
By light microscopy, small vessels adjacent to the areas of scarring were the most common abnormality. Vessel density was significantly higher in operated sclera compared to normal, healthy tissue, regardless of the type of implant used. The average vessel densities were 2.18±1.48 vessels/mm 2 in non-implanted sclera, 2.34±1.69 vessels/mm 2 in eyes with absorbable implants, and 3.64±1.78 vessels/mm 2 in eyes with non-absorbable implants. Analysis of iron distribution in ferritin-injected eyes showed a positive reaction inside new aqueous draining vessels in all groups. TEM analysis showed that the ultrastructure of new vessels matched the features of the small veins.
Conclusions
Aqueous outflow after NPDS can be achieved through the newly formed network of small intrascleral veins. Use of non-absorbable implants significantly increases vessel density in the sclera adjacent to implanted material compared to eyes in which absorbable implants or no implants were used.
Related collections
Most cited references18
- Record: found
- Abstract: found
- Article: not found
Reducing capsular thickness and enhancing angiogenesis around implant drug release systems.
- Record: found
- Abstract: found
- Article: not found
Comparative study between deep sclerectomy with and without collagen implant: long term follow up.
- Record: found
- Abstract: found
- Article: not found
