- Record: found
- Abstract: found
- Article: found
Gastric Bypass and Abdominal Pain: Think of Petersen Hernia
Read this article at
Abstract
A “swirl sign” on computerized tomography is an indicator of internal herniation through Petersen’s space and should prompt immediate diagnostic laparoscopy in patients following laparoscopic Roux-en-Y gastric bypass.
Abstract
Background:
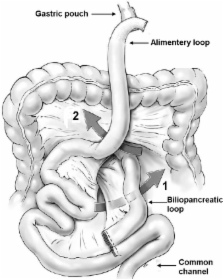
Laparoscopic Roux-en-Y gastric bypass (LRYGB) is one of the most commonly performed bariatric surgical procedures. A laparoscopic gastric bypass is associated with specific complications: internal herniation is one of these.
Case Report:
A 47-year-old woman had undergone a laparoscopic Roux-en-Y gastric bypass (LRYGB) 18 months before presentation at our emergency department with mild abdominal complaints. Physical examination showed signs of an ileus in the absence of an acute abdomen. Laboratory investigations revealed no abnormalities (CRP 2.0 mg/L, white blood count 6.3 × 109/L). During admission, there was clinical deterioration on the third day. Emergency laparotomy was performed. An internal herniation through Petersen's space was found that strangulated and perforated the small bowel. A resection with primary anastomosis and closure of the defects was performed.
Conclusion:
Diagnosing an internal herniation through Petersen's space is difficult due to the nonspecific clinical presentation. The interpretation of the CT scan poses another diagnostic challenge. This sign is present in 74% of the cases with this herniation. A missed diagnosis of internal herniation may cause potentially serious complications. A patient with a gastric bypass who experiences intermittent abdominal complaints should undergo laparoscopy to rule out internal herniation.
Related collections
Most cited references10
- Record: found
- Abstract: found
- Article: not found
Internal hernia after gastric bypass: sensitivity and specificity of seven CT signs with surgical correlation and controls.
- Record: found
- Abstract: found
- Article: not found
Small bowel obstruction and internal hernias after laparoscopic Roux-en-Y gastric bypass.
- Record: found
- Abstract: found
- Article: not found