- Record: found
- Abstract: found
- Article: found
Circadian patterns of heart rate, respiratory rate and skin temperature in hospitalized COVID-19 patients
Read this article at
Abstract
Rationale
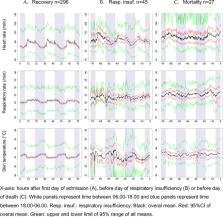
Vital signs follow circadian patterns in both healthy volunteers and critically ill patients, which seem to be influenced by disease severity in the latter. In this study we explored the existence of circadian patterns in heart rate, respiratory rate and skin temperature of hospitalized COVID-19 patients, and aimed to explore differences in circadian rhythm amplitude during patient deterioration.
Methods
We performed a retrospective study of COVID-19 patients admitted to the general ward of a tertiary hospital between April 2020 and March 2021. Patients were continuously monitored using a wireless sensor and fingertip pulse oximeter. Data was divided into three cohorts: patients who recovered, patients who developed respiratory insufficiency and patients who died. For each cohort, a population mean cosinor model was fitted to detect rhythmicity. To assess changes in amplitude, a mixed-effect cosinor model was fitted.
Results
A total of 429 patients were monitored. Rhythmicity was observed in heartrate for the recovery cohort (p<0.001), respiratory insufficiency cohort (p<0.001 and mortality cohort (p = 0.002). Respiratory rate showed rhythmicity in the recovery cohort (p<0.001), but not in the other cohorts (p = 0.18 and p = 0.51). Skin temperature also showed rhythmicity in the recovery cohort (p<0.001), but not in the other cohorts (p = 0.22 and p = 0.12). For respiratory insufficiency, only the amplitude of heart rate circadian pattern increased slightly the day before (1.2 (99%CI 0.16–2.2, p = 0.002)). In the mortality cohort, the amplitude of heart rate decreased (-1.5 (99%CI -2.6- -0.42, p<0.001)) and respiratory rate amplitude increased (0.72 (99%CI 0.27–1.3, p = 0.002) the days before death.
Conclusion
A circadian rhythm is present in heart rate of COVID-19 patients admitted to the general ward. For respiratory rate and skin temperature, rhythmicity was only found in patients who recover, but not in patients developing respiratory insufficiency or death. We found no consistent changes in circadian rhythm amplitude accompanying patient deterioration.
Related collections
Most cited references46
- Record: found
- Abstract: found
- Article: not found
Dexamethasone in Hospitalized Patients with Covid-19 — Preliminary Report
- Record: found
- Abstract: found
- Article: not found
Neurologic Manifestations of Hospitalized Patients With Coronavirus Disease 2019 in Wuhan, China

- Record: found
- Abstract: found
- Article: found