- Record: found
- Abstract: found
- Article: found
Cytokine Release Syndrome Associated with T-Cell-Based Therapies for Hematological Malignancies: Pathophysiology, Clinical Presentation, and Treatment
Read this article at
Abstract
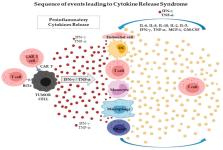
Cytokines are a broad group of small regulatory proteins with many biological functions involved in regulating the hematopoietic and immune systems. However, in pathological conditions, hyperactivation of the cytokine network constitutes the fundamental event in cytokine release syndrome (CRS). During the last few decades, the development of therapeutic monoclonal antibodies and T-cell therapies has rapidly evolved, and CRS can be a serious adverse event related to these treatments. CRS is a set of toxic adverse events that can be observed during infection or following the administration of antibodies for therapeutic purposes and, more recently, during T-cell-engaging therapies. CRS is triggered by on-target effects induced by binding of chimeric antigen receptor (CAR) T cells or bispecific antibody to its antigen and by subsequent activation of bystander immune and non-immune cells. CRS is associated with high circulating concentrations of several pro-inflammatory cytokines, including interleukins, interferons, tumor necrosis factors, colony-stimulating factors, and transforming growth factors. Recently, considerable developments have been achieved with regard to preventing and controlling CRS, but it remains an unmet clinical need. This review comprehensively summarizes the pathophysiology, clinical presentation, and treatment of CRS caused by T-cell-engaging therapies utilized in the treatment of hematological malignancies.
Related collections
Most cited references92
- Record: found
- Abstract: found
- Article: found
COVID-19: consider cytokine storm syndromes and immunosuppression
- Record: found
- Abstract: found
- Article: not found
Tisagenlecleucel in Children and Young Adults with B-Cell Lymphoblastic Leukemia
- Record: found
- Abstract: found
- Article: not found