- Record: found
- Abstract: found
- Article: found
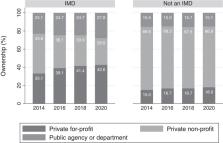
Changes in institution for mental diseases (IMD) ownership status and insurance acceptance over time
Read this article at
Abstract
State Medicaid programs are prohibited from using federal dollars to pay institutions for mental diseases (IMDs)—freestanding psychiatric facilities with more than 16 beds. Increasingly, regulatory mechanisms have made payment of treatment in these settings substantially more feasible. This study evaluates if changing financial incentives are associated with increases in for-profit ownership among IMD facilities relative to non-IMD facilities, as well as greater increases in Medicaid acceptance among for-profit IMD facilities relative to for-profit non-IMD facilities. We used data from the 2014–2020 National Mental Health Services Surveys and examined 11 945 facility-years. Relative to non-IMDs, the increase in for-profit ownership among IMDs was 6.6 percentage points greater. The largest proportional change in Medicaid acceptance occurred among for-profit IMD facilities relative to for-profit non-IMDs (18.5 percentage points). Existing research is mixed on the quality of inpatient and residential psychiatric care provided in for-profit vs nonprofit and public facilities, as well as in IMD relative to non-IMD facilities. As payment policy increasingly incentivizes for-profit facilities to enter the psychiatric care space, we should be mindful of the impact of these decisions on patient safety.
Related collections
Most cited references18
- Record: found
- Abstract: found
- Article: not found
Changes in Quality of Care after Hospital Mergers and Acquisitions
- Record: found
- Abstract: not found
- Article: not found
Health Care Market Concentration Trends In The United States: Evidence And Policy Responses
- Record: found
- Abstract: not found
- Article: not found