- Record: found
- Abstract: found
- Article: found
Factors influencing post-ICU psychological distress in family members of critically ill patients: a linear mixed-effects model
Read this article at
Abstract
Background
Adverse responses to critical illness, such as symptoms of depression, anxiety or posttraumatic stress, are relatively common among family members. The role of risk factors, however, remains insufficiently understood, but may be important to target those family members most in need for support. We therefore examined the association of patient-, family member- and care-related factors with post-ICU psychological distress in family members in a general population of critical ill patients.
Methods
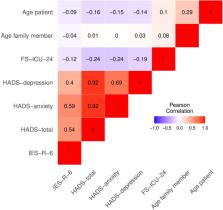
We conducted a prospective, single-centre observational study in a twelve-bed surgical ICU in a 900-bed University Hospital in Switzerland. Participants were family members of patients treated in ICU who completed the Family Satisfaction in ICU-24 Survey, the Hospital Anxiety Depression Scale, Impact of Event Scale-Revised-6, and a demographic form within the first 3 months after their close other’s ICU stay. Data were analysed using linear mixed-effects models, with depression, anxiety, and posttraumatic stress as outcome measures.
Results
A total of 214 family members (53% return rate) returned a completed questionnaire. We found that higher levels of satisfaction were significantly associated with lower levels of depression, anxiety and posttraumatic stress. There was no statistically significant association between family member characteristics and any measure of psychological distress. Among the included patient characteristics, younger patient age was associated with higher levels of depression, and patient death was associated with higher levels of depression and posttraumatic stress.
Conclusions
Our results suggest that satisfaction with ICU care is strongly associated with family well-being post-ICU. Family members of younger patients and of those who die seem to be most at risk for psychological distress, requiring specific support, whereas family member characteristics may have less relevance.
Related collections
Most cited references51
- Record: found
- Abstract: found
- Article: not found
The validity of the Hospital Anxiety and Depression Scale. An updated literature review.
- Record: found
- Abstract: found
- Article: not found
Guidelines for Family-Centered Care in the Neonatal, Pediatric, and Adult ICU.
- Record: found
- Abstract: found
- Article: not found