- Record: found
- Abstract: found
- Article: found
A Pilot Study of Application of the Stroke Riskometer Mobile App for Assessment of the Course and Clinical Outcomes of COVID-19 among Hospitalized Patients
Abstract
Introduction
Early determination of COVID-19 severity and health outcomes could facilitate better treatment of patients. Different methods and tools have been developed for predicting outcomes of COVID-19, but they are difficult to use in routine clinical practice.
Methods
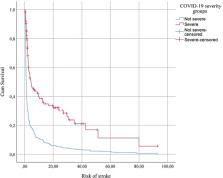
We conducted a prospective cohort study of inpatients aged 20–92 years, diagnosed with COVID-19 to determine whether their individual 5-year absolute risk of stroke at the time of hospital admission predicts the course of COVID-19 severity and mortality. The risk of stroke was determined by the Stroke Riskometer mobile application.
Results
We examined 385 patients hospitalized with COVID-19 (median age 61 years). The participants were categorized based on COVID-19 severity: 271 (70.4%) to the “not severe” and 114 (29.6%) to the “severe” groups. The median risk of stroke the next day after hospitalization was significantly higher among patients in the severe group (2.83, 95% CI: 2.35–4.68) versus the not severe group (1.11, 95% CI: 1.00–1.29). The median risk of stroke and median systolic blood pressure (SBP) were significantly higher among non-survivors (12.04, 95% CI: 2.73–21.19) and (150, 95% CI: 140–170) versus survivors (1.31, 95% CI: 1.14–1.52) and (134, 95% CI: 130–135), respectively. Those who spent more than 2.5 h a week on physical activity were 3.1 times more likely to survive from COVID-19. Those who consumed more than one standard alcohol drink a day, or suffered with atrial fibrillation, or had poor memory were 2.5, 2.3, and 2.6 times more likely not to survive from COVID-19, respectively.
Related collections
Most cited references22
- Record: found
- Abstract: not found
- Article: not found
Nonparametric Estimation from Incomplete Observations
- Record: found
- Abstract: found
- Article: not found
Epidemiology, clinical course, and outcomes of critically ill adults with COVID-19 in New York City: a prospective cohort study
- Record: found
- Abstract: found
- Article: not found